J Res Clin Med. 12:7.
doi: 10.34172/jrcm.32220
Original Article
Frequency of dry eye syndrome in patients with multiple sclerosis: A cross-sectional case-control study
Rana Sorkhabi Conceptualization, Funding acquisition, Validation, Writing – original draft, 1 
Siamak Khavandi Formal analysis, Methodology, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing, 1, * 
Hormoz Ayromlou Data curation, Validation, 2
Mohammad Hosein Ahoor Resources, 1
Mehdi Mohammadkhani Project administration, Writing – review & editing, 1
Elsa Tabibzadeh Investigation, Visualization, 3
Author information:
1Department of Ophthalmology, Tabriz University of Medical Sciences, Tabriz, Iran
2Department of Neurology, Tabriz University of Medical Sciences, Tabriz, Iran
3Department of Anesthesiology and Intensive Care, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Introduction:
Demyelination of the nerve fibers of the central nervous system is a main pathology of multiple sclerosis (MS), in which inflammation plays a major role. Studies have shown that inflammation is the leading cause of dry eye disorder. To investigate the association between inflammation and both diseases, we aimed to estimate the prevalence of dry eye syndrome (DES) in MS patients and its correlation with the severity of the disease and disability status.
Methods:
We enrolled 100 MS patients randomly and 100 healthy controls. DES was evaluated by Dry Eye questionnaire and Scoring System (DESS), tear break-up time (TBUT), tear meniscus height (TMH), and Schirmer 1 & 2 tests in subjects. Furthermore, the leading disability in MS was assessed by a clinician (neurology professor) using the related questionnaire (Expanded Disability Status Scale).
Results:
According to the TBUT, THM, and Schirmer tests, the number of subjects with abnormal results was significantly higher in the MS group than in the control group. The severity of DES measured by the DESS was also higher in the MS group compared to control group. Also, there was a significant relationship between increasing disability and abnormal dry eye tests, especially in MS patients with EDSS scores>4.
Conclusion:
The present study highlights the importance of considering dry eye disorder in MS patients as a possible consequence of inflammation. Also, our results suggested a significant relationship between dry eye disorder and the EDSS scores.
Keywords: Dry eye disorder, Multiple sclerosis, Inflammation, Schirmer
Copyright and License Information
© 2024 The Authors.
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
This study was funded by Tabriz University of Medical Sciences as a thesis for the residency program (Thesis No. 60500).
Introduction
Multiple sclerosis (MS) involves the entire central nervous system, causing neurological disability of varying levels due to its demyelinating nature. The incidence and prevalence of MS are increasing worldwide. However, the underlying cause of this remains uncertain.1 Another known culprit in MS pathogenesis is the change in patients’ immune system. The main immune-pathogenesis of MS is related to the overexpression of T-helper 1 (Th1) and Th17 activity, whose function is to secretion of pro-inflammatory cytokines. It also appears that the activity of regulatory T (Treg) cells and Th2 cells, which normally control inflammation, is reduced during the course of the disease.2 MS induces many pathological mechanisms that generate a wide range of symptoms, from other autoimmune-related diseases and disorders to various eye-related complications, including optic neuritis, diplopia, uveitis, and visual field defects.3 One particular field that has been gravely overlooked by both ophthalmologists and immunologists is the effect of MS on tear layers and lacrimal glands, causing mild to severe Keratoconjunctivitis sicca.
The tear film is composed of three layers: the mucous layer (or inner layer), the aqueous layer (or middle layer), and the lipid layer (or outer layer).4 The main and accessory lacrimal glands such as Krause, are responsible for secreting the thicker aqueous layer, which is watery and forms the main part of the tear.5 The slightest anomaly or deformity in any tear layers could lead to instability of the tear film and development of dry eyes symptoms. Dry eye disorder is relatively common in the community, affecting the overall quality of life by causing continuous discomfort and serious damage to the eye surface. An inflammatory response is one of the known mechanisms involved in the occurrence of the dry eye disorder.6,7
Multiple studies have been conducted on ocular findings in MS patients, but little research has been done in the field of ocular surface changes. Particularly, few studies have been conducted on the function of the lacrimal system, which report a decrease in tear secretion as a side effect in some patients with MS. A recent investigation indicated that patients with the primary progressive form of MS had a higher prevalence of abnormal Schirmer test results compared to the general population.8
In the present study, we performed lacrimal system function tests and utilized the Dry Eye Scoring System (DESS), a validated tool, 9 to determine the frequency of this disorder in patients with MS and assess the correlation between its various stages. The DESS questionnaire is provided in Table S1 (Supplementary file 1). Most of the articles on the effect of MS on the eye focus on the disease’s impact on visual changes, optic neuritis, ocular movement disorders, nystagmus and uveitis. However, there is insufficient data on MS causing dry eye syndrome (DES). In the course of our study, we endeavor to compensate for the apparent lack of research in the latter field by conducting a novel research that investigates the manifestations of dry eye disorder in MS patients.
Methods
In our study, conducted at Nikoukari hospital (affiliated with Tabriz University of Medical Sciences, Tabriz, Iran); with the approval of the ethics committee (Code: IR.TBZMED.REC.1398.454), MS patients were enrolled and data pool of the two main MS clinics of the city was used. After explaining the study’s core elements, we enrolled patients, and those willing to participate signed a consent form. The target population included adults ( > 18 years old) with confirmed MS who were under 60 years old and the statistical sample was selected randomly using a simple randomization method by giving the cases a specific code and choosing among them using random digits table. The number of the cases at each step of the sample selection is shown in Figure 1. Controls were recruited from patients’ companions in other wards who were eager to participate.
Figure 1.
Sample selection
.
Sample selection
Exclusion criteria were using contact lenses, using medications that affect the tear film during the past month, history of trauma, diabetes, ocular infections, decreased corneal sensation, trigeminal nerve dysfunction, systemic conditions that could exacerbate dry eye, history of refractive surgery in the eye, ocular surface abnormalities with other causes, consciousness and psychological disorders and allergy to fluorescein. Participants were asked to avoid using eye drops or ointments for one week prior to the examination.
First, a questionnaire was filled out, which included patient information, age, sex, type, and duration of treatment, as well as DESS questionnaire. The questionnaire consisted of six items with a score range of 0 to 3. The questions covered issues regarding itching, redness, blurred vision, fatigue of the eye, the need for frequent blinking, and the sensation of a foreign sandy object in the eye. The final score ranged from 0 to 18, with 0-6 indicating mild dry eye, 6-12 indicating moderate dry eye, and 12-18 indicating the presence of severe dry eye disorder. Regarding age and gender, each control group shared the same attributes as its respective test group.
All patients were subsequently examined by the same certified ophthalmologist and supervised by the same cornea fellow, with an exclusive focus on the right eye. This was followed by a number of diagnostic tests, including tear break-up time (TBUT) and Schirmer 1& 2 tests. To minimize the possibility of errors or biases in the study, the right eyes were chosen for examination. The rationale behind choosing only the right eye of each patient is that both eyes of an individual might not be exposed to the same amount of sunlight (a risk factor for tear evaporation) during daily activities like driving (due to the left side driving seat).
TBUT test: First, we poured single drop of 2% sodium fluorescein solution into the lower conjunctival sac to examine the stability of tear layer. Then we recorded the time from right after blinking until the presence of the first hints of black dots in the lacrimal film. Times less than ten seconds was considered abnormal.
Schirmer 1 & 2 tests: These tests were performed to estimate the quantitative output and tear flow on the surface of each eye, both with and without anesthesia, using Schirmer paper strip. We folded the strips and placed them in the outer third of the inferior fornix. When inserting the strip, the patient was asked to look upward for the next 5 minutes. After the allocated time, the moistened part of the strip was measured. Depending on the absence or presence of topical anesthesia (Schirmer 1 and Schirmer 2 respectively), moisture levels below ten and five millimeters were considered abnormal, respectively. The same type of Schirmer paper strips were used for all participants.
Tear meniscus height (TMH) test: We used fluorescein for staining the tear meniscus. Then, the maximum height of the tear meniscus above the lower eyelid edge was measured, and the results of less than 0.3 mm were considered abnormal.
Currently, we do not have a diagnostic gold standard for dry eye evaluation. Considering this fact, we measured the scores for each test and compared them between the two groups independently, both in terms of mean and percentage of abnormal test results after applying the cutoff points.
Finally, we used Expanded Disability Status Scale (EDSS) to determine the disability status of disease in MS patients. This tool has an ordinal grading system ranging from 0 (normal status of neurologic system) to 10 (MS caused death) in 0.5 increments.
Results
We investigated the lacrimal gland status and activity in MS compared to normal people as controls, and the results are given in Table 1.
Table 1.
Comparison of dry eye test results for study groups (MS and Control groups), ranges are shown in parentheses
|
Test
|
Control group
|
MS group
|
P
value
|
| Schirmer test 1 (mm) |
15.2 ± 4.6 (4-22) |
12.2 ± 4.1 (3-20) |
0.01* |
| Schirmer test 2 (mm) |
10.1 ± 4.4 (2-19) |
7.8 ± 3.7 (1-14) |
0.01* |
| TMH (mm) |
0.5 ± 0.2 (0.1-0.8) |
0.4 ± 0.1 (0.1-0.6) |
0.02* |
| DESS |
2.6 ± 2.1 (0-14) |
4.7 ± 3.5 (0-16) |
0.01* |
| TBUT (s) |
14.5 ± 4.6 (5-23) |
11.0 ± 5.3 (3-25) |
0.01* |
TMH, Tear meniscus height; TBUT, tear break up time; DESS, Dry Eye questionnaire and Scoring System.
* Fisher exact test.
We applied the commonly used cutoff points of the previous studies to investigate the frequency of DES in both groups. According to TBUT, TMH, and Schirmer tests, the number of subjects with abnormal results was significantly higher in the MS group compared to the control group. Schirmer 1 test was abnormal in 35% of MS group, indicating a high frequency of dry eye disease. Likewise, abnormal TMH and TBUT test results were higher in MS patients (32% and 37%, respectively) (Figure 2).
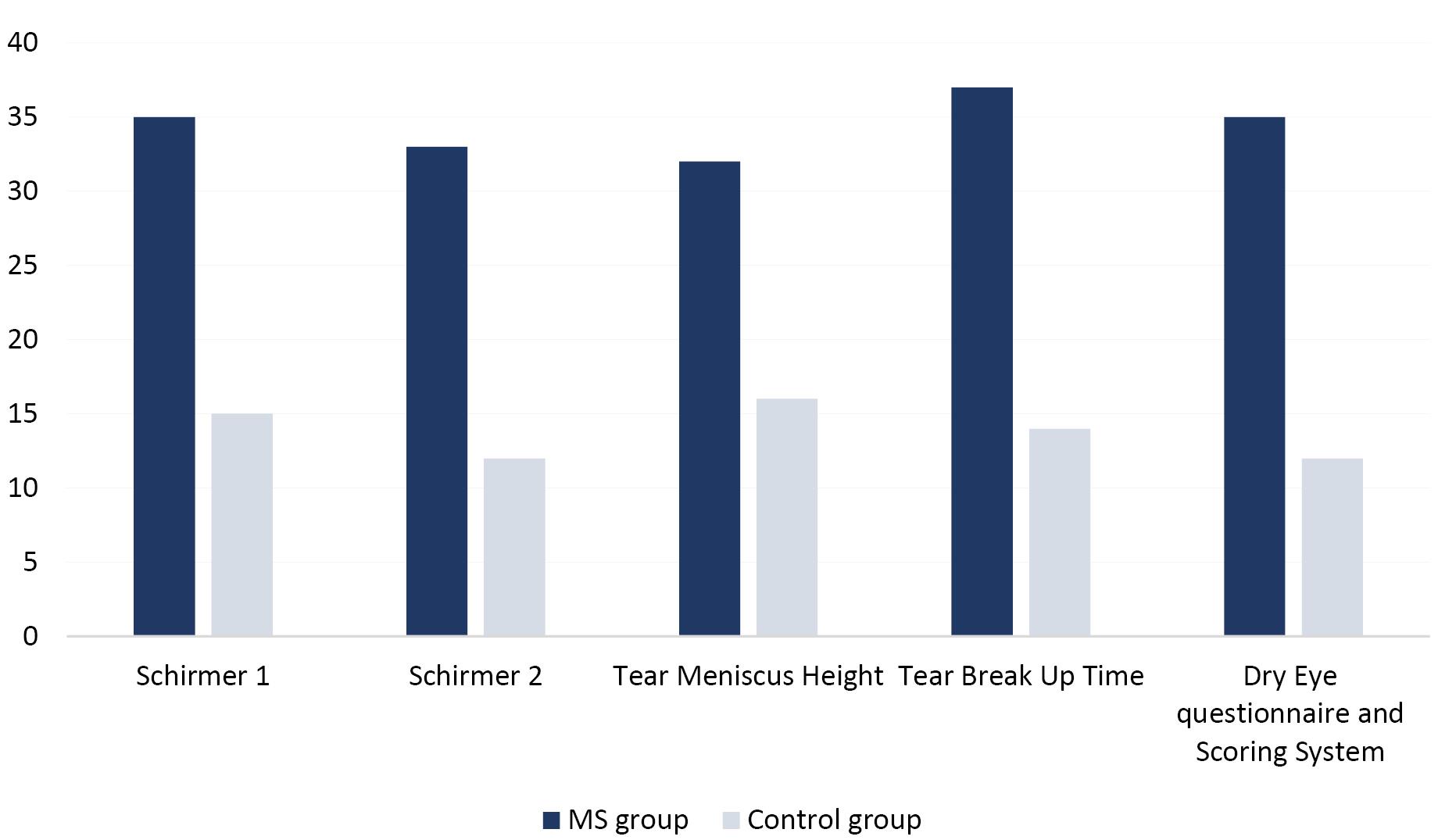
Figure 2.
Percentage of abnormal tests indicating dry eye in MS & control group (P < 0.05)
.
Percentage of abnormal tests indicating dry eye in MS & control group (P < 0.05)
DESS severity was similarly higher in the MS group compared to the control group. The number of individuals with mild dry eye was substantially lower in the MS group than in the control group (Table 2). Also, there was a significant relationship between increasing disability and abnormal dry eye tests, especially in MS patients with EDSS scores > 4 (Spearman’s rank correlation test).
Table 2.
Dry Eye questionnaire and Scoring System (DESS) results in terms of dry eye severity for study groups (MS and control groups)
|
|
MS group
|
Control group
|
P
value
|
| DESS |
Symptom-free |
54 |
69 |
0.02 |
| Mild |
11 |
19 |
0.01 |
| Moderate |
28 |
10 |
0.01 |
| Severe |
7 |
2 |
0.01 |
Discussion
The current study was designed and implemented to identify and assess the dry eye prevalence in MS patients compared to normal controls. DES is a status that can be present in a healthy population with a prevalence of 5%-17%. Some studies on Sjogren syndrome and Rheumatoid arthritis reported the prevalence of dry eye about 23 per 1000 person-years.10,11
MS disease pathogenesis has integral parts of the inflammatory cytokines secreted by Th1 and Th17, resulting in increased blood-brain barrier permeability to monocytes and macrophages. Th1 cells are found in damaged parts of the CNS and are actively present in MS patients’ bloodstream, which produces inflammatory cytokines.12,13 Inflammatory reactions are one of the known mechanisms in the occurrence of dry eyes. In the more severe forms of dry eyes, the level of inflammatory cytokines is higher than normal in the conjunctival epithelium.14,15 Our result showed that significantly 46% of MS patients were symptomatic based on DESS evaluation consequences. Also, the severity of symptoms was more elevated in MS group than in the healthy people (4.7 ± 3.5 vs. 2.6 ± 2.1; P = 0.01). Considering the inflammatory condition in patients with MS due to the nature of the disease, we can expect that these patients will be symptomatic compared to the control group based on DESS evaluations. Consistent with our study, Belviranli et al reported higher dry eye subjective and objective symptoms and conjunctival impression cytology abnormalities (such as goblet cell loss and conjunctival squamous metaplasia with high grades) in MS involved patients. For this reason, ophthalmologists should monitor MS patients for ocular surface changes, especially DES.16
The ocular surface is capable of responding to various stimuli in and out of the body and thereby modulating immune responses to avert the negative aspects of the inflammatory response. According to the latest research, dry eye is characterized as a localized autoimmune ailment that arises from impaired immune-modulatory and pro-inflammatory responses.17 Normally, the cornea is short of both blood vessels and lymphatic that in turn bring on its angiogenic privileges. These characteristics prevent cells that presenting antigen (also called APCs) from trafficking to the lymphatic tissues and gives the anterior part of the eye an important immune privilege property.18 Anti-inflammatory factors such as regulatory T cells (Treg) on the ocular surface and tears decrease the pro-inflammatory factors produced by APCs following ocular surface stimulation.19
In our MS patients, the value of Schirmer tests 1 (12.2 ± 4.1 vs. 15.2 ± 4.6 mm; P = 0.01) and 2 (7.8 ± 3.7 mm vs. 10.1 ± 4.4 mm; P = 0.01) were significantly lower than healthy controls. Also, the TMH significantly lower in MS group than in the controls (0.4 ± 0.1 mm vs. 0.5 ± 0.2 mm; P = 0.02). Consisted of recent study showed that the mean Schirmer 1 test result was significantly lower in MS group than in the controls (8.45 ± 5.75 mm vs. 17.36 ± 10.89 mm; P < 0.001).16
Dry eye disease exacerbates the following alterations in Tregs immune-modulatory features.20 On the other hand, Th1 and Th17 cells that elevate proinflammatory responses, have an important role in MS pathogenesis as well. Inflammation also induces goblet cells loss and disrupts the tear integrity.21 Similarly, our results showed that the TBUT was lower in MS group than in the controls and this is significant (11.0 ± 5.3 s vs. 14.5 ± 4.6 s; P = 0.01); which shows that patients with MS suffer from dry eyes. Guannan et al also reported DES in patients with autoimmune diseases can be a common manifestation of disease.22
The tear in patients suffering from dry eye disease can become hyperosmolar, and ocular surface exposure to hyperosmolar tear also leads to oxidative stress and cell cycle disruption.23 Then, a signaling cascade provoked by protein kinase activation (that was activated by mitogen) and upregulates various pro-inflammatory mediators and causes inflammation on the ocular surface that accelerates maturation of APCs.24 Recent studies indicated that Th1 and Th17 cells make several cytokines (especially pro-inflammatory) and lead to corneal barrier disturbance, corneal angiogenesis, and loss of goblet cells.25
The primary type of DES is related to meibomian gland dysfunction (MGD) which comes from dysfunction of the tear glands that produce the lipid layer, which maintains the consistency of the tear film. Considering that MGD prevalence is much higher in older people, the target population of our study was limited to 60 years old to reduce the interference of MGD on the data.
We found a significant association between the frequency of DES and severity of disability in MS group. To our knowledge, in this study we evaluated the dryness of eyes in MS patients regarding the severity of their condition for the first time and further studies need to be conducted in this field. Our study had certain limitations, including the lack of measurement of tear osmolarity in MS patients. Another major limitation of the study was the inability/unwillingness of some MS patients with severe disability to cooperate with fluorescein staining of the cornea/conjunctiva as a diagnostic test of dry eye disease. Further studies are also recommended in MS patients to measure inflammatory markers.
Our results indicate that dry eye is a prevalent pathological condition in MS patients. Additionally, there is a significant connection between dry eyes and the disability rate in MS patients, with the aggravation of dry eyes in more severe levels of disability.
Study Highlights
What is current knowledge?
-
Multiple sclerosis is a chronic autoimmune disorder affecting the central nervous system. It involves the immune system attacking the protective covering of nerve fibers, leading to disrupted communication between the brain and other parts of the body.
-
There is a growing body of research suggesting a potential link between multiple sclerosis and dry eye syndrome.
What is new here?
Conclusion
Since dry eye imposes a heavy burden on patients and their quality of life, dry eye disease symptoms should be noticed early during diagnosis, and further ophthalmic examinations should be recommended.
Acknowledgments
We would like to thank Dr. Rahul Bhargava for granting us permission to use DESS questionnaire in our study.
Competing Interests
All authors declare that they have no conflicts of interest.
Ethical Approval
This research was conducted under the ethical supervision of ethics committee of TBZMED (Code: IR.TBZMED.REC.1398.454).
Supplementary File
Supplementary file 1 contaion Table S1.
(pdf)
References
- Browne P, Chandraratna D, Angood C, Tremlett H, Baker C, Taylor BV. Atlas of multiple sclerosis 2013: a growing global problem with widespread inequity. Neurology 2014; 83(11):1022-4. doi: 10.1212/wnl.0000000000000768 [Crossref] [ Google Scholar]
- Comabella M, Khoury SJ. Immunopathogenesis of multiple sclerosis. Clin Immunol 2012; 142(1):2-8. doi: 10.1016/j.clim.2011.03.004 [Crossref] [ Google Scholar]
- Solaro C, Trabucco E, Messmer Uccelli M. Pain and multiple sclerosis: pathophysiology and treatment. Curr Neurol Neurosci Rep 2013; 13(1):320. doi: 10.1007/s11910-012-0320-5 [Crossref] [ Google Scholar]
- Willshire C, Buckley RJ, Bron AJ. Central connections of the lacrimal functional unit. Cornea 2017; 36(8):898-907. doi: 10.1097/ico.0000000000001250 [Crossref] [ Google Scholar]
- Sack RA, Beaton A, Sathe S, Morris C, Willcox M, Bogart B. Towards a closed eye model of the pre-ocular tear layer. Prog Retin Eye Res 2000; 19(6):649-68. doi: 10.1016/s1350-9462(00)00006-9 [Crossref] [ Google Scholar]
- Messmer EM. The pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch Arztebl Int 2015; 112(5):71-81. doi: 10.3238/arztebl.2015.0071 [Crossref] [ Google Scholar]
- Fiscella RG. Understanding dry eye disease: a managed care perspective. Am J Manag Care 2011; 17 Suppl 16:S432-9. [ Google Scholar]
- de Seze J, Devos D, Castelnovo G, Labauge P, Dubucquoi S, Stojkovic T. The prevalence of Sjögren syndrome in patients with primary progressive multiple sclerosis. Neurology 2001; 57(8):1359-63. doi: 10.1212/wnl.57.8.1359 [Crossref] [ Google Scholar]
- Bhargava R, Rajpoot M, Arora Y, Sharma SK, Sharma S. Dietary omega-3 fatty acids supplements for dry eye in psoriasis: are they effective? molecules. J Clin Diagn Res 2017; 11(11):NC01-5. doi: 10.7860/jcdr/2017/27490.10799 [Crossref] [ Google Scholar]
- Barrientos RT, Godín F, Rocha-De-Lossada C, Soifer M, Sánchez-González JM, Moreno-Toral E. Ophthalmological approach for the diagnosis of dry eye disease in patients with Sjögren’s syndrome. Life (Basel) 2022; 12(11):1899. doi: 10.3390/life12111899 [Crossref] [ Google Scholar]
- Lai SC, Wang CW, Wu YM, Dai YX, Chen TJ, Wu HL. Rheumatoid arthritis associated with dry eye disease and corneal surface damage: a nationwide matched cohort study. Int J Environ Res Public Health 2023; 20(2):1584. doi: 10.3390/ijerph20021584 [Crossref] [ Google Scholar]
- Salehi M, Bagherpour B, Shayghannejad V, Mohebi F, Jafari R. Th1, Th2 and Th17 cytokine profile in patients with multiple sclerosis following treatment with rapamycin. Iran J Immunol 2016; 13(2):141-7. [ Google Scholar]
- Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 2018; 17(2):162-73. doi: 10.1016/s1474-4422(17)30470-2 [Crossref] [ Google Scholar]
- Stern ME, Pflugfelder SC. Inflammation in dry eye. Ocul Surf 2004; 2(2):124-30. doi: 10.1016/s1542-0124(12)70148-9 [Crossref] [ Google Scholar]
- Pflugfelder SC. Antiinflammatory therapy for dry eye. Am J Ophthalmol 2004; 137(2):337-42. doi: 10.1016/j.ajo.2003.10.036 [Crossref] [ Google Scholar]
- Belviranli S, Oltulu P, Uca AU, Gundogan AO, Mirza E, Altas M. Conjunctival impression cytology and tear film parameters in patients with multiple sclerosis. Int Ophthalmol 2022; 42(2):593-600. doi: 10.1007/s10792-021-02031-5 [Crossref] [ Google Scholar]
- Stevenson W, Chauhan SK, Dana R. Dry eye disease: an immune-mediated ocular surface disorder. Arch Ophthalmol 2012; 130(1):90-100. doi: 10.1001/archophthalmol.2011.364 [Crossref] [ Google Scholar]
- Li S, Li L, Zhou Q, Gao H, Liu M, Shi W. Blood vessels and lymphatic vessels in the cornea and iris after penetrating keratoplasty. Cornea 2019; 38(6):742-7. doi: 10.1097/ico.0000000000001922 [Crossref] [ Google Scholar]
- Tepelus TC, Chiu GB, Huang J, Huang P, Sadda SR, Irvine J. Correlation between corneal innervation and inflammation evaluated with confocal microscopy and symptomatology in patients with dry eye syndromes: a preliminary study. Graefes Arch Clin Exp Ophthalmol 2017; 255(9):1771-8. doi: 10.1007/s00417-017-3680-3 [Crossref] [ Google Scholar]
- Ratay ML, Glowacki AJ, Balmert SC, Acharya AP, Polat J, Andrews LP. Treg-recruiting microspheres prevent inflammation in a murine model of dry eye disease. J Control Release 2017; 258:208-17. doi: 10.1016/j.jconrel.2017.05.007 [Crossref] [ Google Scholar]
- Chen Y, Chauhan SK, Shao C, Omoto M, Inomata T, Dana R. IFN-γ-expressing Th17 cells are required for development of severe ocular surface autoimmunity. J Immunol 2017; 199(3):1163-9. doi: 10.4049/jimmunol.1602144 [Crossref] [ Google Scholar]
- Guannan H, Long S, Xia H, Dong W, Shaozhen Z. Clinical characterisation and cytological study of dry eye in patients with autoimmune disease. J Pak Med Assoc 2018; 68(3):353-8. [ Google Scholar]
- Aguilar A, Berra A. Hyperosmolarity of the tear film in the dry eye. In: Kopacz D, ed. Ocular Surface Diseases-Some Current Date on Tear Film Problem and Keratoconic Diagnosis. IntechOpen; 2020.
- Acosta MC. Ocular thermography in ocular inflammation and dry eye. Acta Ophthalmol 2019;97(S263). 10.1111/j.1755-3768.2019.5004.
- Rhee MK, Mah FS. Inflammation in dry eye disease: how do we break the cycle?. Ophthalmology 2017; 124(11s):S14-9. doi: 10.1016/j.ophtha.2017.08.029 [Crossref] [ Google Scholar]