J Res Clin Med. 12:29.
doi: 10.34172/jrcm.34623
Original Article
Investigating predictors in parenteral to oral switch of Analgesia in postoperative patients: An observational study
Sandhya Y Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, * 
Hafsa Sami Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 
Clint Joe Kanjamala Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 
Swetha Gopan Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 
Author information:
Department of Pharmacy Practice, Bapuji Pharmacy College, Shamanur Road, S S Layout, Davangere- 577004, Karnataka, India
Abstract
Introduction:
A thorough understanding of various routes of analgesic administration and their limitations enables pain therapists to effectively manage postoperative pain, reduce the risk of chronic pain development, and enhance patient satisfaction. Considerations such as pain type, patient preferences and medical conditions guide the selection of the most appropriate administration method and dosage form for optimal outcomes. This observational study aimed to investigate the factors associated with the switch of analgesic medication from parenteral to oral in postoperative patients.
Methods:
This study was conducted for six months among 305 patients at a tertiary care teaching hospital, Davangere, India. The data about patient was collected through case sheets and was analyzed with IBM SPSS Version 25 for windows.
Results:
The study conducted on 305 patients found that the switch was mostly done within the time interval of 2-4 days. The combination of paracetamol and tramadol (22.6%) was the main drug of choice for switch. The switch from parenteral to oral analgesia was not found to be significantly associated with age, severity of pain, or length of hospital stay.
Conclusion:
Although switching between parenteral and oral routes of analgesic administration appears to be effective in managing surgical patients, but the decision to switch does not seem to be influenced by the hypothesized factors.
Keywords: Analgesics, Oral, Pain management, Parenteral, Postoperative
Copyright and License Information
© 2024 The Authors.
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
No funding source to be declare.
Introduction
Postoperative pain management intends to enhance patient satisfaction and promote optimal recovery.1,2 The intensity of postoperative pain is considered a significant risk factor for the development of persistent postsurgical pain.3 Ensuring appropriate postoperative analgesia will lower the occurrence of persistent postsurgical pain, hospitalization duration, readmissions, and complications.4-7
The right administration method and dosage form must be selected while initiating analgesics to get the best results. When deciding on the most appropriate route for administering pain medication, several factors come into play. These factors encompass the type of pain experienced, its intensity and location, the preferences of the patient, and their specific medical conditions. In addition, it is crucial to consider the speed at which the analgesic takes effect, the duration of its action, how easily it can be administered, patient adherence to the treatment plan, and the associated costs.8
Traditionally, severely ill or following surgery, patients in hospitals often start receiving their medications intravenously and then orally.9 Epidural analgesia is considered more effective than intravenous opioid analgesics and it is recommended for the high-risk patients undergoing thoracic, upper abdominal, and lower limb surgery. Moreover, it is found to be superior in reducing pain and less likely to cause adverse effects such as nausea and vomiting, while also promoting patient mobility.8,10,11
Transition from intravenous to oral administration of analgesics, is often overlooked in the hospital setting despite its benefits in terms of patient comfort, reduced nursing workload, and potentially shorter hospital stays.12-14 A deeper understanding of the diverse routes of administering analgesics, as well as their indications and limitations can greatly support pain therapists in delivering optimal acute pain management and proactively averting the onset of chronic pain.15 The prospective cross sectional observational study was carried out to identify analgesic switch to investigate the factors which may influence with the switch of analgesic medication from parenteral to oral in postoperative patients.
Methods
This study was conducted for six months from March 2022 to August 2022 at Shamnur Shivashankarappa Institute of Medical Sciences & Research Center, a tertiary care teaching hospital, Davangere, India. The study population included patients above the age of 18 who underwent surgery, prescribed with at least one analgesic and received parenteral analgesics on initial therapy. We excluded patients with psychiatric disorders and who refused to give consent. In view of all the inclusion and exclusion criteria, 305 patients were selected from postoperative wards of general surgery and orthopaedics.
Materials used
Materials used in the study were predesigned consent form and data collection form. For assessing pain intensity, standard numerical rating scale (NRS-11) was used. Informed consent was taken from each patient before enrollment. The data about patient was collected through case sheets and the pain score was assessed from patient’s response to NRS-11 on postoperative day 1, day 3 and on discharge. Medication charts were reviewed. The obtained data was documented in data collection form and analysed.
Statistical analysis
The sample size was calculated using the G*Power software version 3.9.7. Categorical data was represented in the form of frequency and percentage. Association between variables was assessed with chi-square test. Quantitative data was represented as Mean and Standard. Inter Group comparison of variables was done with unpaired t test. Intra Group comparison of variables has been done with Paired t test. To find out the relation between variables Pearson’s Correlation was used. P value of < 0.05 was considered statistically significant. Data was analyzed with IBM Statistical Package for Social Sciences (SPSS, version 25) on Windows.
Results
The study included a total of 305 participants, with 201 undergoing general surgery and 104 from the orthopaedics department. Among the participants, 131 were female and 174 were male, with mean age of 47.27 years.
Following surgery, the patients reported experiencing pain at various time intervals. 279 patients (91.4%) experienced pain within 24 hours, while 15 patients (5%) complained of pain between 24 to 48 hours. Only three patients (1%) perceived pain after 48 hours, and eight patients (2.6%) reported no pain at all.
When pain intensity was measured on day 1 of surgery, 220 patients (72.1%) had severe pain, 62 patients (20.4%) moderate pain, nine patients (3%) mild pain and 14 patients (4.5%) had no pain. The intensity of pain was severe in majority of patients.
The study population received different pattern of analgesic therapy. Either single analgesic treatment or more than one analgesic was given. 135 patients (44.3%) were treated with monotherapy and 170 of them (55.7%) received multidrug therapy through three different methods. The intravenous (IV) route was the most preferred method, with 263 patients (84%) receiving medication this way. For 39 patients (12.5%), a combination of IV and oral administration was used. Additionally, three patients (0.95%) received analgesics via the epidural route.
Figure 1 depicts the analgesics prescribed parenterally for initial therapy. Paracetamol (37.97%) was the most commonly used drug followed by tramadol (35.02%). During the course of treatment, patients receiving parenteral analgesia eventually transitioned to oral therapy. Among them, 173 (56.7%) patients were switched to oral medication, while 132 (43.2%) patients remained on parenteral therapy throughout their hospitalization. A significant number of patients (68.2%) underwent the transition from parenteral to oral medication within a relatively short period of 2 to 4 days. Following this, 24.3% of patients were switched to oral therapy within 5 to 7 days. A smaller subset of patients was shifted to oral analgesics at a later stage, as shown in Figure 2. The combination of paracetamol and tramadol (22.6%) was the main drug of choice after switch of analgesics. The other drugs used are presented in Figure 3.
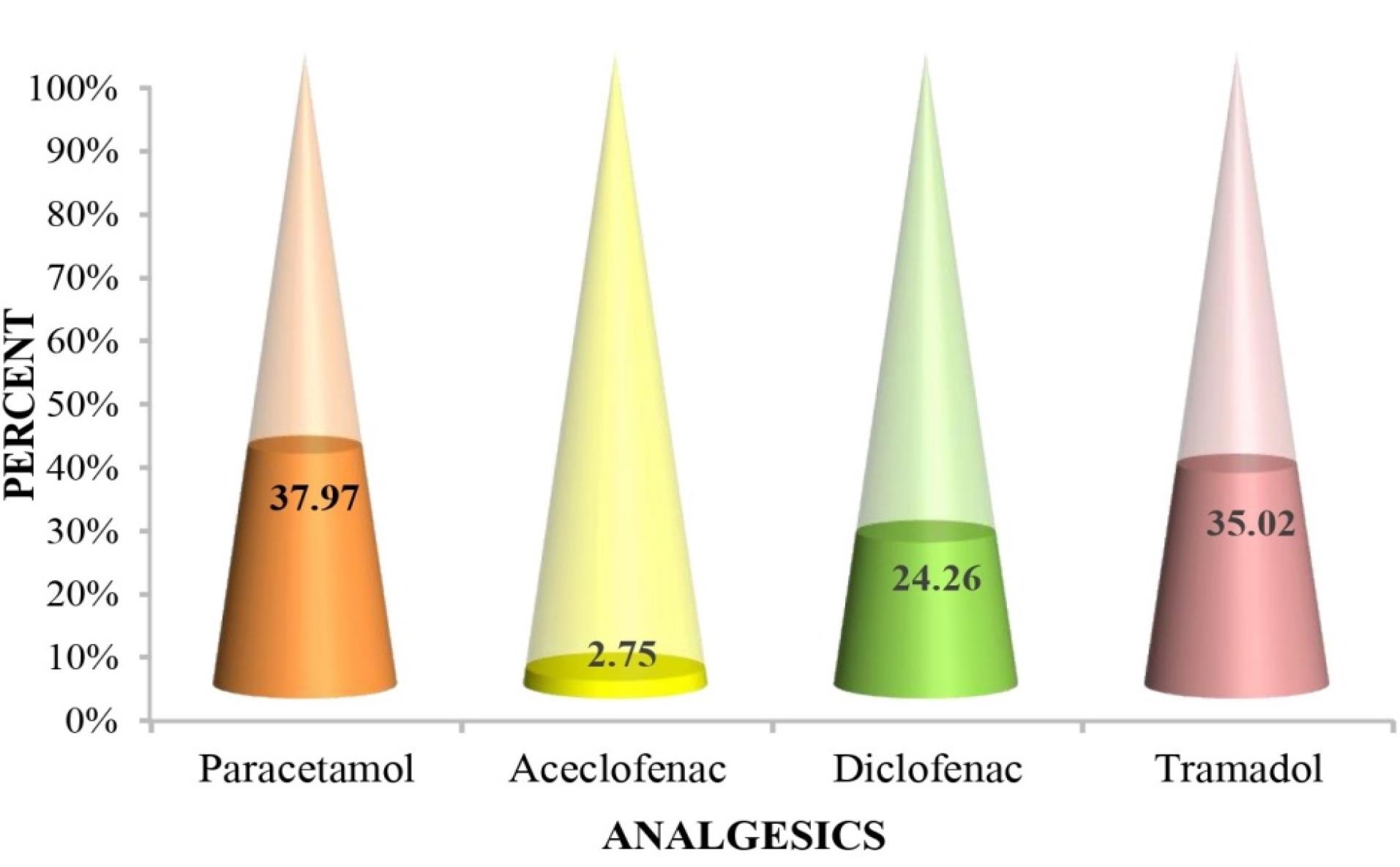
Figure 1.
Parenteral Analgesics prescribed
.
Parenteral Analgesics prescribed
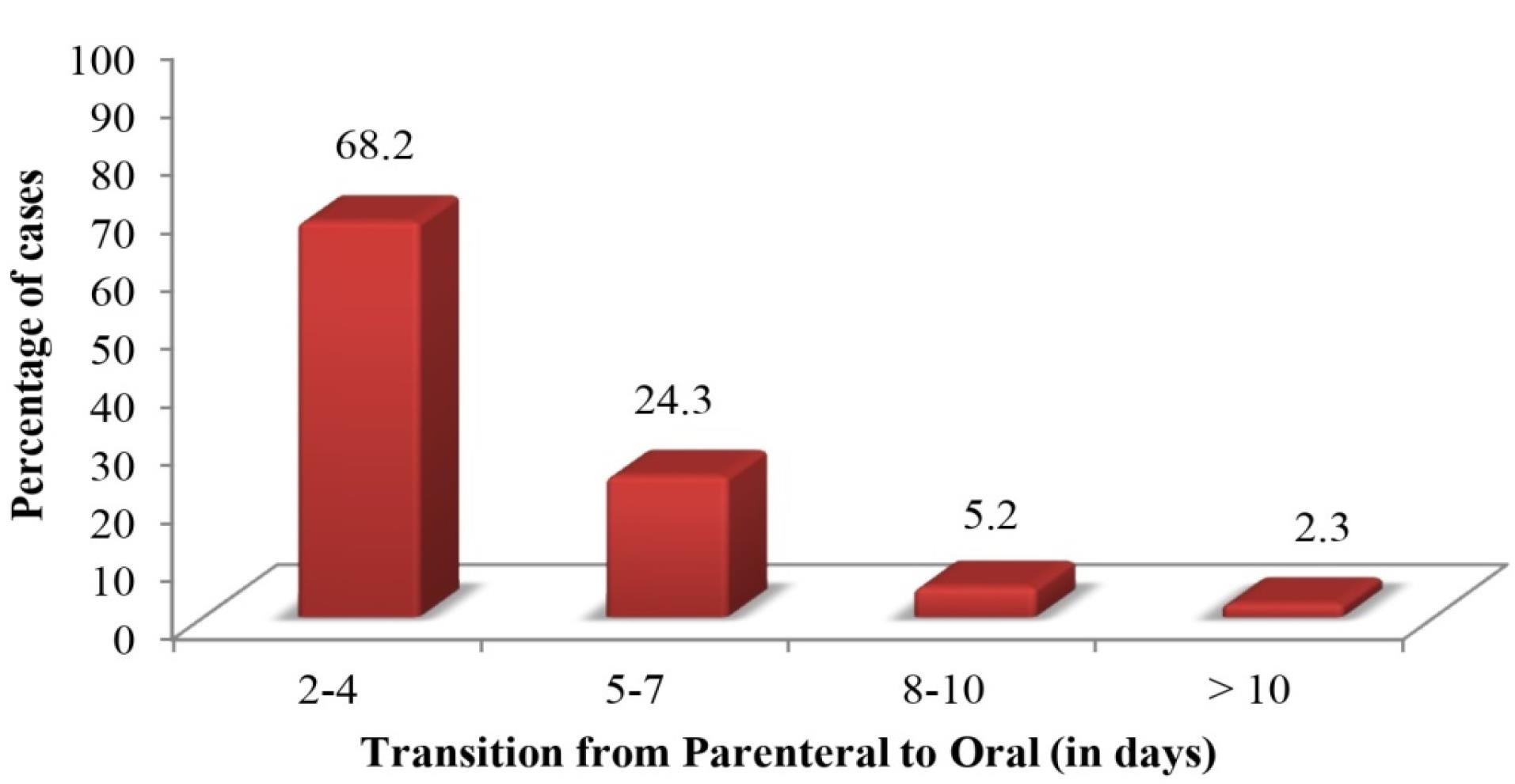
Figure 2.
Time taken for parenteral to oral switch
.
Time taken for parenteral to oral switch
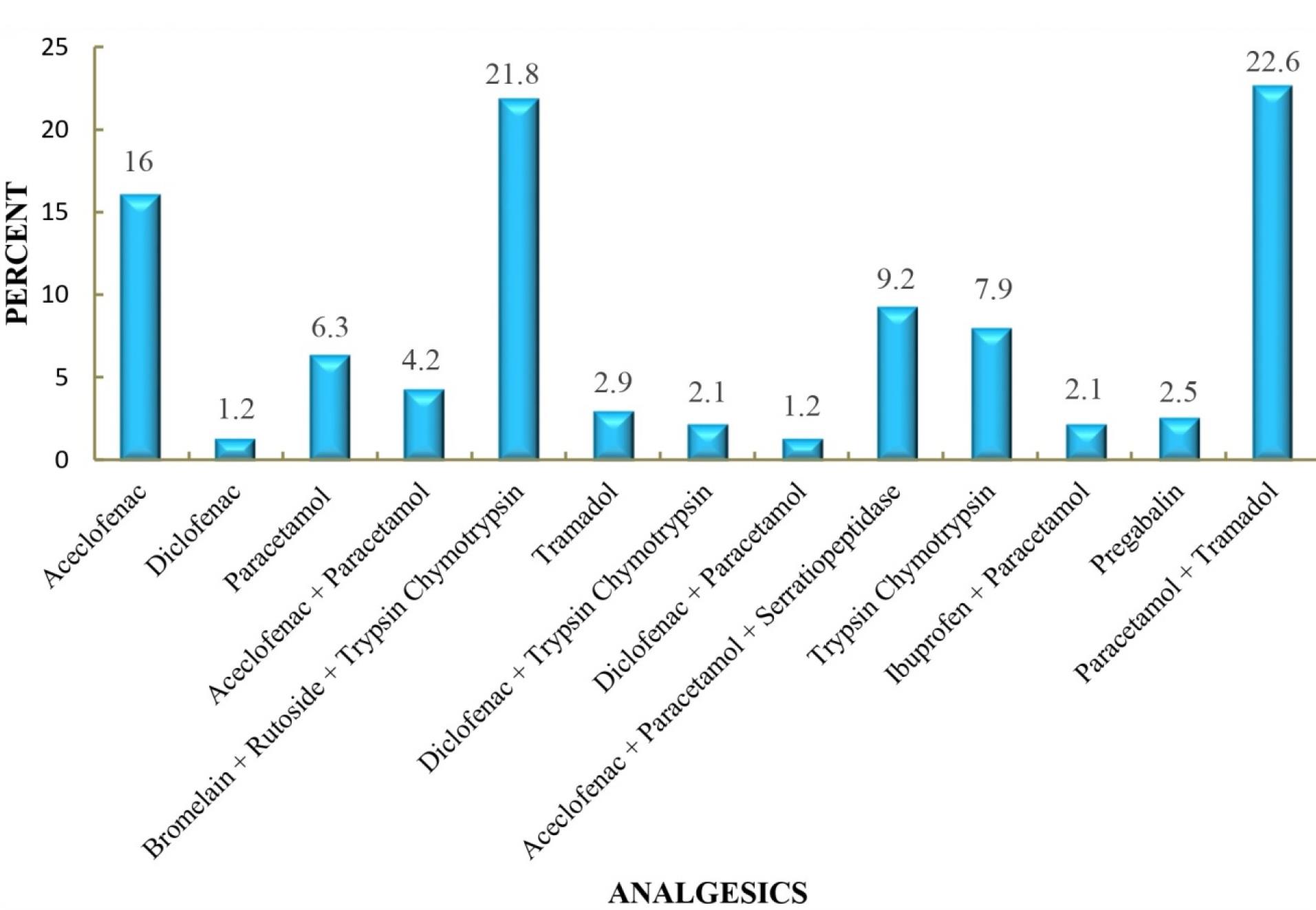
Figure 3.
Medications used in parenteral to oral switch
.
Medications used in parenteral to oral switch
We hypothesized that several factors might contribute to the switch from parenteral to oral analgesics. However, observing our cases, it was suspected that age, pain severity and hospital stay might have influenced this decision. Thus we investigated the potential associations between age, pain severity, and the length of hospital stay with the decision to switch the route of analgesic administration.
The individuals who underwent switch from parenteral to oral analgesic were divided into different age groups in Table 1. A statistical analysis was performed to assess the relationship between the switch and patient age, revealing a P value of 0.237. This finding suggests that there is no significant association between the age of the patient and the decision to switch the route of analgesic therapy. As the pain intensity was measured on the third day, a significant proportion experienced considerably reduced pain at this time, that is, moderate pain (41.6%) to severe pain (40.5%). Majority of patients (68.2%) underwent the switch to oral therapy within the same period of 2-4 days. However, as the patients approached the time of discharge, the severity of pain had been considerably diminished and all the participants had been transitioned to oral therapy. The statistical association between the switch and pain intensity yielded P values of 0.364 for third day and 0.424 for the discharge day. Consequently, the results indicate a lack of association between the severity of pain and the decision to switch analgesics. Thus, Table 2 data suggest that the decision to switch to oral therapy was independent of the level of pain intensity. Table 3 compares the duration of hospital stay and the switch of analgesic therapy. Among the patients included in the analysis, a majority (57.8%) had a hospital stay ranging from 8 to 14 days, while only a small percentage (1.1%) of those had a stay exceeding 28 days. As observed, the P value of 0.167 indicates that patient’s length of hospital stay was not influenced by whether the patient underwent analgesic switch or not. Therefore, there was no statistically significant association between the switch of analgesic therapy and the duration of hospital stay.
Table 1.
Cross tabulation of age and parenteral to oral switch
|
Age
|
Parenteral to Oral Switch
|
|
Yes
|
No
|
|
Number of cases
|
%
|
Number of cases
|
%
|
| 18-20 |
11 |
6.3 |
4 |
3 |
| 21-30 |
29 |
16.8 |
22 |
16.7 |
| 31-40 |
25 |
14.5 |
24 |
18.2 |
| 41-50 |
27 |
15.6 |
28 |
21.2 |
| 51-60 |
45 |
26 |
19 |
14.4 |
| 61-70 |
26 |
15 |
26 |
19.7 |
| > 70 |
10 |
5.8 |
9 |
6.8 |
| Total |
173 |
100 |
132 |
100 |
Chi-square test, P = 0.237
Table 2.
Severity of pain and parenteral to oral switch
|
Severity of pain
|
Parenteral to oral switch
|
|
3rd day of surgerya
|
Day of dischargeb
|
|
Yes
|
No
|
Yes
|
No
|
|
Number of cases
|
%
|
Number of cases
|
%
|
Number of cases
|
%
|
Number of cases
|
%
|
| Mild |
30 |
17.3 |
18 |
13.6 |
114 |
65.9 |
73 |
55.3 |
| Moderate |
72 |
41.6 |
47 |
35.6 |
39 |
22.5 |
40 |
30.3 |
| Severe |
70 |
40.5 |
62 |
46.9 |
5 |
2.9 |
3 |
2.2 |
| No pain |
1 |
0.6 |
5 |
3.7 |
15 |
8.7 |
16 |
12.1 |
aChi-square test, P = 0.364.
bChi-square test, P = 0.424.
Table 3.
Hospital stay and parenteral to oral switch
|
Hospital stay in days
|
Parenteral to oral switch
|
|
Yes
|
No
|
|
Number of cases
|
%
|
Number of cases
|
%
|
| ≤ 7 |
49 |
28.3 |
59 |
44.6 |
| 8 -14 |
100 |
57.8 |
57 |
43.1 |
| 15 - 21 |
18 |
10.4 |
12 |
9 |
| 22 - 28 |
4 |
2.3 |
3 |
2.2 |
| > 28 |
2 |
1.1 |
1 |
0.75 |
| Total |
173 |
100 |
132 |
100 |
Chi-square test, P = 0.167
Discussion
The selection of the most suitable analgesics is influenced not only by the drug class but also by the most appropriate route of administration, the optimal dosage, and individual patient considerations. The various routes of administration can impact the onset of time, the peak effectiveness, the duration of action, and the dosage needed compared to the parenteral route. The oral route is a favourable choice due to its efficacy, simplicity, and cost-effectiveness. On the other hand, the intravenous route offers rapid onset and easier titration, making it suitable for acute pain management. Epidural analgesia has gained widespread acceptance as a preferred method for treating acute pain during surgical procedures. In our study, all three routes of administration were employed as part of the initial therapy, wherein significant number of participants received intravenous analgesia and in a negligible number of patients epidural analgesia was used. According to Shang and Gan,16 and Puntillo et al,17 administering oral medications immediately after surgery is generally unsuitable for patients who have undergone general anesthesia. This is due to the potential for impaired consciousness and postoperative nausea and vomiting, which could lead to aspiration. If the oral route is used too soon before normal gastric motility returns, the “dumping effect” occurs which may cause elevated risk of adverse events due to accumulated doses.15,16
According to our results paracetamol and tramadol were almost equally used for initial prescription. But the study conducted by Jahr et al and Groudine et al, they concluded that IV acetaminophen is an effective and safe alternative to opioid-based analgesia for acute pain.18,19 In contrast, the study conducted by Erdogan Kayhan et al revealed that intravenous ibuprofen was well tolerated with no serious side effects.20
While changing from intravenous to oral therapy may not be suitable for critically ill patients or those with impaired oral medication absorption, most hospitals will encounter eligible patients for this switch. IV administration is deep-routed to increased adverse effects, such as cannula-related infections, thrombophlebitis, restricted mobility, and delayed discharge. When a patient’s gastrointestinal tract is functioning, and they can tolerate oral formulations, IV administration becomes unnecessary as stated by Jibril et al.21 We found that the switch was mostly done within the time interval of 2-4 days whereas in Marcotte et al study the IV fluids were discontinued within 24 hours.15 The combination of paracetamol and tramadol was the main drug of choice for switch. Before switch, the study population received limited analgesics, including non-steroidal anti-inflammatory drugs (NSAIDs) and tramadol. However, after the switch, a wide range of analgesic adjuvants, such as proteolytic enzymes and anticonvulsants, were also administered.
Our observational study has shed light on the factors which may influence the switch of analgesic medications from parenteral to oral in postoperative patients. There was no significant association between switch of analgesics to any of the following factors: age, severity of pain or length of hospital stay. However, Houchens et al study suggested that IV to oral switch programs can be an effective way to reduce hospital stay without compromising patient outcomes.22 Enhanced recovery protocols in colorectal surgery focus on reducing hospital stay and emphasize on non-opioid multimodal approaches.23 Ultimately, the decision to switch from parenteral to oral medication should be made on a case-by-case basis, taking into account the individual patient’s medical history, pain management needs, and preferences. As per our knowledge there are not many studies conducted to justify the rationalized switching of analgesics. Implementation of newer technology such as patient controlled analgesia (PCA) may provide more effective pain management. A Cochrane Review found that IV opioid PCA showed greater analgesic effectiveness and higher patient satisfaction scores compared to conventional IV “as needed” opioid administration, establishing it as a safer method.23 Overall, this study highlights the importance of considering individual patient conditions when making decisions about analgesic switching and there is need for further research to optimize pain management in postoperative patients.
Limitation of the study
Despite our study had large sample size, there were few short comes such as its observational nature, enhanced generalizability of surgery, limited exploration of potential factors impacting pain management and reliance on self-reported pain scores susceptible for bias.
Study Highlights
What is current knowledge?
What is new here?
-
Parenteral to Oral Shift: Half of the patients had a transition from parenteral to oral analgesic administration during their treatment, while the other half continued parenteral therapy until discharge.
-
Timing of Switch: Although there was variation in the timing of the switch between patients, the majority underwent the transition within a relatively short time span.
-
Factors Not Influencing the Switch: Age, pain intensity, and length of hospital stay were hypothesized to influence the decision to switch, but none were found to be significant factors in this decision.
-
Pain Reduction: Pain intensity consistently decreased from the day of surgery to discharge, regardless of whether or not the patients switched from parenteral to oral analgesics.
-
Optimized Pain Management: Overall, the analgesic therapy was effective and optimized for managing pain, regardless of the administration route.
Conclusion
Out of all participants half of them had parenteral to oral shift of analgesic administration while the other half were not switched till inpatient therapy. Although there were a lot of variations between patients for time taken to switch but most patients underwent switch within a short span. None of the hypothesised factors: Age, intensity of pain and the length of hospital stay contributed the decision to switch. The intensity of pain gradually reduced from day of surgery to discharge irrespective of switch. Overall, the therapy was optimised for pain management.
Acknowledgements
We would like to express our sincere gratitude to Dr. Ann Elizabeth George, Dr. L S Patil, statistician Samshada Begum and professors of Pharmacy Practice Department.
Competing Interests
The authors declare no conflict of interest.
Ethical Approval
This study was approved by the institutional Research Ethics Committee Bapuji Pharmacy College, in a meeting held on March 14th 2022, as recorded in act number BPC/IEC/79/2021-22.
Informed Consent
Consent was taken from each patient. Data sets are kept confidential and available with the corresponding author.
References
- Mallama M, Valencia A, Rijs K, Rietdijk WJ, Klimek M, Calvache JA. A systematic review and trial sequential analysis of intravenous vs oral peri-operative paracetamol. Anaesthesia 2021; 76(2):270-6. doi: 10.1111/anae.15163 [Crossref] [ Google Scholar]
-
American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2012;116 (2):248-73. 10.1097/ALN.0b013e31823c1030.
- Luo J, Min S. Postoperative pain management in the postanesthesia care unit: an update. J Pain Res 2017; 10:2687-98. doi: 10.2147/jpr.s142889 [Crossref] [ Google Scholar]
- Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg 2003; 97(2):534-40. doi: 10.1213/01.ane.0000068822.10113.9e [Crossref] [ Google Scholar]
- Perkins FM, Kehlet H. Chronic pain as an outcome of surgery A review of predictive factors. Anesthesiology 2000; 93(4):1123-33. doi: 10.1097/00000542-200010000-00038 [Crossref] [ Google Scholar]
- Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J Pain 2016; 17(2):131-57. doi: 10.1016/j.jpain.2015.12.008 [Crossref] [ Google Scholar]
- Wu CL, Raja SN. Treatment of acute postoperative pain. Lancet 2011; 377(9784):2215-25. doi: 10.1016/s0140-6736(11)60245-6 [Crossref] [ Google Scholar]
- Puntillo F, Giglio M, Varrassi G. The routes of administration for acute postoperative pain medication. Pain Ther 2021; 10(2):909-25. doi: 10.1007/s40122-021-00286-5 [Crossref] [ Google Scholar]
- Sabry N, Dawoud D, Alansary A, Hounsome N, Baines D. Evaluation of a protocol-based intervention to promote timely switching from intravenous to oral paracetamol for post-operative pain management: an interrupted time series analysis. J Eval Clin Pract 2015; 21(6):1081-8. doi: 10.1111/jep.12463 [Crossref] [ Google Scholar]
- National Institute for Health and Care Excellence. Perioperative care in adults. NICE Guideline: Methods NG180. NICE; 2020.
- Schug SA, Palmer GM, Scott DA, Alcok M, Halliwell R, Mott J. APM: SE Working Group of the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine, Acute Pain Management: Scientific Evidence. 5th ed. Melbourne: ANZCA & FPM; 2020.
- Vanstraelen K, Verhaegen J, Peetermans WE, Willems L, Spriet I. Stimulation of the IV to oral switch of bioavailable drugs by phone calls in a Belgian tertiary care hospital. Acta Clin Belg 2013; 68(3):179-82. doi: 10.2143/acb.3212 [Crossref] [ Google Scholar]
- Mertz D, Koller M, Haller P, Lampert ML, Plagge H, Hug B. Outcomes of early switching from intravenous to oral antibiotics on medical wards. J Antimicrob Chemother 2009; 64(1):188-99. doi: 10.1093/jac/dkp131 [Crossref] [ Google Scholar]
- McLaughlin CM, Bodasing N, Boyter AC, Fenelon C, Fox JG, Seaton RA. Pharmacy-implemented guidelines on switching from intravenous to oral antibiotics: an intervention study. QJM 2005; 98(10):745-52. doi: 10.1093/qjmed/hci114 [Crossref] [ Google Scholar]
- Marcotte JH, Patel KM, Gaughan JP, Dy J, Kwiatt ME, McClane SJ. Oral versus intravenous acetaminophen within an enhanced recovery after surgery protocol in colorectal surgery. Pain Physician 2020; 23(1):57-64. [ Google Scholar]
- Shang AB, Gan TJ. Optimising postoperative pain management in the ambulatory patient. Drugs 2003; 63(9):855-67. doi: 10.2165/00003495-200363090-00002 [Crossref] [ Google Scholar]
- Puntillo F, Giglio M, Varrassi G. The routes of administration for acute postoperative pain medication. Pain Ther 2021; 10(2):909-25. doi: 10.1007/s40122-021-00286-5 [Crossref] [ Google Scholar]
- Jahr JS, Filocamo P, Singh S. Intravenous acetaminophen: a review of pharmacoeconomic science for perioperative use. Am J Ther 2013; 20(2):189-99. doi: 10.1097/MJT.0b013e31828900cb [Crossref] [ Google Scholar]
- Groudine S, Fossum S. Use of intravenous acetaminophen in the treatment of postoperative pain. J Perianesth Nurs 2011; 26(2):74-80. doi: 10.1016/j.jopan.2010.11.001 [Crossref] [ Google Scholar]
- Erdogan Kayhan G, Sanli M, Ozgul U, Kirteke R, Yologlu S. Comparison of intravenous ibuprofen and acetaminophen for postoperative multimodal pain management in bariatric surgery: a randomized controlled trial. J Clin Anesth 2018; 50:5-11. doi: 10.1016/j.jclinane.2018.06.030 [Crossref] [ Google Scholar]
- Jibril F, Sharaby S, Mohamed A, Wilby KJ. Intravenous versus oral acetaminophen for pain: systematic review of current evidence to support clinical decision-making. Can J Hosp Pharm 2015; 68(3):238-47. doi: 10.4212/cjhp.v68i3.1458 [Crossref] [ Google Scholar]
- Houchens N, Lele AV, Padgett JM. The association between IV to PO conversion program and hospital length of stay: a systemic review and meta-analysis. J Hosp Med 2016; 11(12):862-7. [ Google Scholar]
- Garimella V, Cellini C. Postoperative pain control. Clin Colon Rectal Surg 2013; 26(3):191-6. doi: 10.1055/s-0033-1351138 [Crossref] [ Google Scholar]