J Res Clin Med. 12:30.
doi: 10.34172/jrcm.33460
Original Article
Predictors of recurrent ischemic stroke: A retrospective cohort study
Sheida Shaafi Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 1, * 
Yalda Sadeghpour Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing, 1 
Zahra Masroor Data curation, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing, 2
Seyed Aria Nejadghaderi Investigation, Methodology, Writing – original draft, Writing – review & editing, 3, 4 
Author information:
1Neurosciences Research Center (NSRC), Tabriz University of Medical Sciences, Tabriz, Iran
2Department of Neurology, Tabriz Branch, Islamic Azad University, Tabriz, Iran
3HIV/STI Surveillance Research Center, and WHO Collaborating Center for HIV Surveillance, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
4Research Center for Integrative Medicine in Aging, Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Introduction:
Cerebrovascular events are one of the most common causes of disability and the third leading cause of death in developed countries. Herein, we aimed to investigate the potential underlying causes of recurrent ischemic stroke.
Methods:
This study was a retrospective cohort study conducted in Razi Hospital, Tabriz, Iran between March 2018 and September 2020. Patients with the diagnosis of recurrent ischemic stroke during the study period were eligible to be included. Baseline characteristics and data on the recurrence were collected using chart reviews. Also, binary logistic regression was used to examine the factors related to recurrence.
Results:
Among one hundred participants with a mean age of 68.88 years, 59% were male. Hypertension, diabetes, heart disease, smoking, and hyperlipidemia were identified in 79%, 42%, 24%, 15%, and 15%, respectively. The average recurrence time of stroke was about 2.52 years. According to our findings, a significant relationship between the history of heart diseases and ischemic stroke recurrence was observed (risk ratio: 0.10: 95% confidence interval: 0.03-0.33).
Conclusion:
We found no significant association between ischemic stroke recurrence and underlying diseases except for heart diseases. Further large-scale observational studies and meta-analyses are recommended to evaluate the possible association.
Keywords: Atherosclerotic disease, Diabetes, Hypertension, Recurrent ischemic stroke, Risk factor
Copyright and License Information
© 2024 The Authors.
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
None.
Introduction
Cerebrovascular diseases are one of the most common neurological conditions associated with high mortality and long-term morbidities.1 Patients who recover from the first stroke events are at higher risk of recurrence, especially within the first two years.2 Moreover, some other comorbidities, including hypertension, diabetes mellitus, atrial fibrillation, and transient ischemic attack are known main risk factors for recurrent form.3 Approximately 80%-85% of patients who experienced a first cerebrovascular accident survived a second event. However, in different communities, around 15%-30% of patients with a history of stroke within the past two years experienced a recurrent stroke.4,5
Compared to the first stroke attack, neurological disorders caused by a recurrent form are more complicated to treat, and have a higher mortality rate, leading to hospital readmission and long-term disability.6 Additionally, the cumulative effects of previous stroke complications should be taken into consideration under these conditions.7 Therefore, secondary prevention is of importance for these individuals.
Previous studies have evaluated the incidence and predictors of stroke in some populations.8,9 Moreover, some systematic review and meta-analyses have calculated the cumulative risk and risk factors for recurrent stroke.6,7,10 Nevertheless, to our best of knowledge, no previous recent study has assessed the predictors of recurrent stroke in Iranian population. So, we aimed to investigate the predictors of recurrent stroke and their presentation in a tertiary center in Northwest of Iran.
Methods
Study design and subjects
In this retrospective cohort study, cluster sampling was used, and 100 patients with recurrent ischemic stroke from March 2018 to September 2020 who re-admitted to Razi Medical Training Center, Tabriz University of Medical Sciences, Tabriz, Iran were enrolled. All patients with the diagnosis of recurrent ischemic stroke during the study period were eligible to be included in the study. The participants should have complete baseline information and agree to participate in the study. The lack of ischemic stroke history and non-ischemic stroke diagnosis were considered exclusion criteria.
Data collection
For demographic characteristics of enrolled individuals with recurrent ischemic stroke, the questionnaire included identification characteristics, hospitalization date, age, gender, underlying diseases (e.g., diabetes mellitus, hypertension, hyperlipidemia, and heart diseases), smoking, family history of cardiovascular or cerebrovascular diseases, age (when the first stroke attack occurred), final diagnosis, complications, and the treatment protocols used for the previous stroke was completed for each patient. The time interval of ischemic stroke recurrence was also calculated based on years and categorized along with defined variables such as age and gender. Finally, the impact of each variable on the recurrence of ischemic stroke was also investigated.
Study outcomes
The primary outcome was to determine the predictors of recurrent ischemic stroke. The secondary outcomes were also to provide the characteristics of patients with recurrent ischemic stroke by considering age, gender, underlying disease, and time interval of ischemic stroke recurrence.
Statistical analysis
The analysis was conducted using the Statistical Package for the Social Sciences (SPSS) version 24 (SPSS Inc., Chicago, IL, USA). To evaluate the normal distribution of variables, the Smirnov-Kolmogorov test was performed. By using descriptive statistical techniques, demographic characteristics were examined and provided with percentages, frequencies, means, and standard deviations (SD). The independent sample T-test or Mann-Whitney U test was also used to analyze quantitative variables. In addition, we used binary logistic regression to explore the relationship between underlying risk factors affecting on stroke recurrence. Statistical significance was considered a p value under 0.05.
Results
Of the 100 patients enrolled in the study, 59% were men and the mean age was 68.88 years (SD: 10.51) (Table 1). The majority of patients were in the age range of 65 to 75 years old (Figure 1). According to data analysis, the frequency of hypertension, diabetes mellitus, heart diseases, smoking, and hyperlipidemia were 79%, 42%, 24%, 15%, and 15%, respectively (Table 1). Moreover, 79 patients experienced recurrent stroke with the average interval time of 3 ± 2 years. While, in 42 patients the period of stroke recurrence was one year or less (Table 1 and Figure 2). Twelve patients had more than one experience of the recurrent ischemic stroke. Notably, the regression model showed a 90% lower risk of recurrent ischemic events in patients without the history of heart diseases (risk ratio [RR]: 0.10; 95% confidence interval [CI]: 0.03-0.33). However, hypertension, diabetes mellitus, hyperlipidemia, smoking, and age did not show a significant effect on the stroke recurrence (Table 2).
Table 1.
Baseline characteristics of participants
|
Variables
|
Number,
mean
|
Percent, standard deviation
|
| Baseline characteristic |
|
|
| Male |
59 |
59% |
| Age, year (mean) |
68.88 |
10.51 |
| Underlying conditions |
|
|
| Hypertension |
79 |
79% |
| Diabetes |
42 |
42% |
| Smoking |
15 |
15% |
| Hyperlipidemia |
15 |
15% |
| Heart diseases |
24 |
24% |
| Time interval of ischemic stroke recurrence |
|
|
| Time interval, year (mean) |
2.52 |
3.34 |
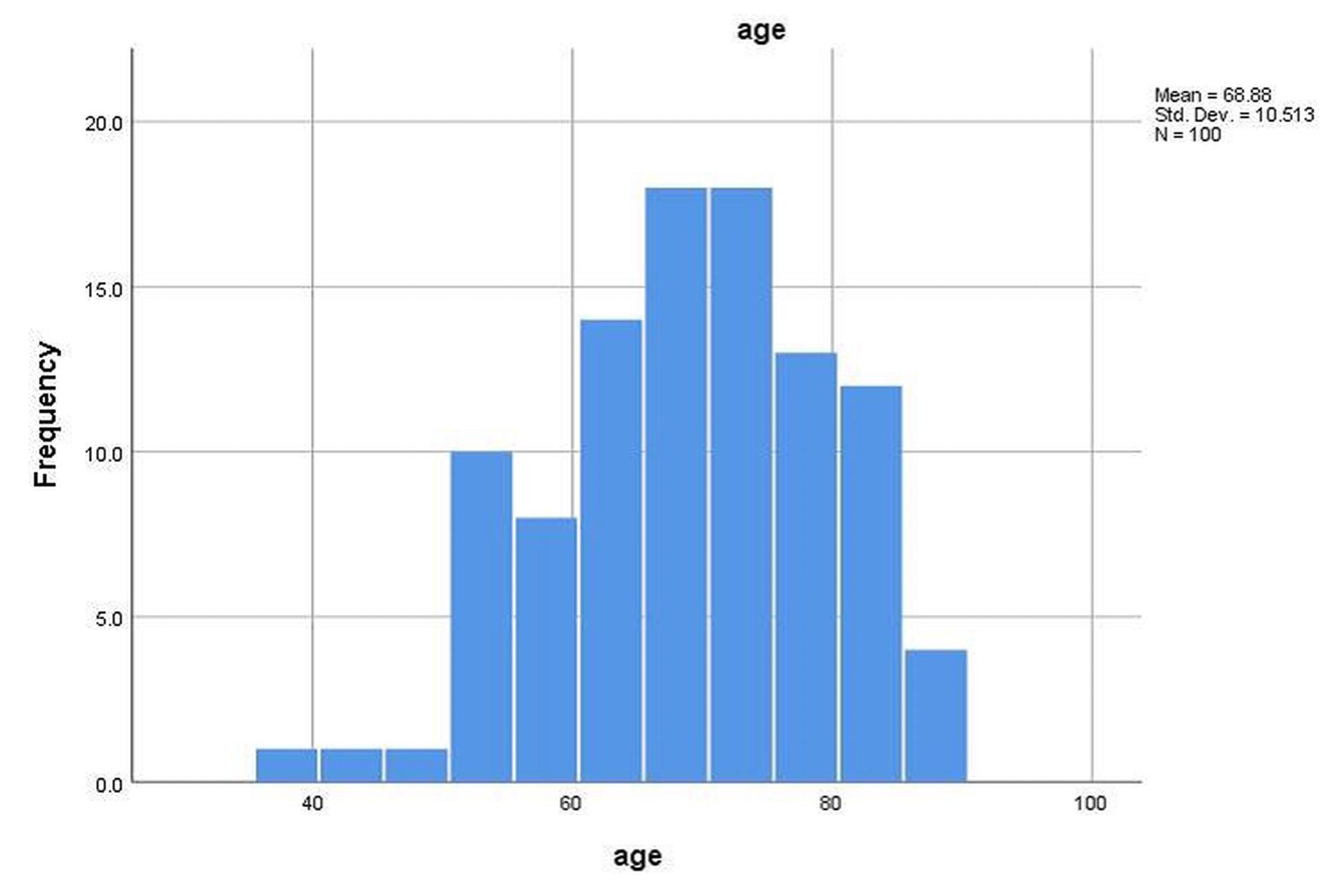
Figure 1.
Age histogram of patients with recurrent ischemic stroke included in the study
.
Age histogram of patients with recurrent ischemic stroke included in the study
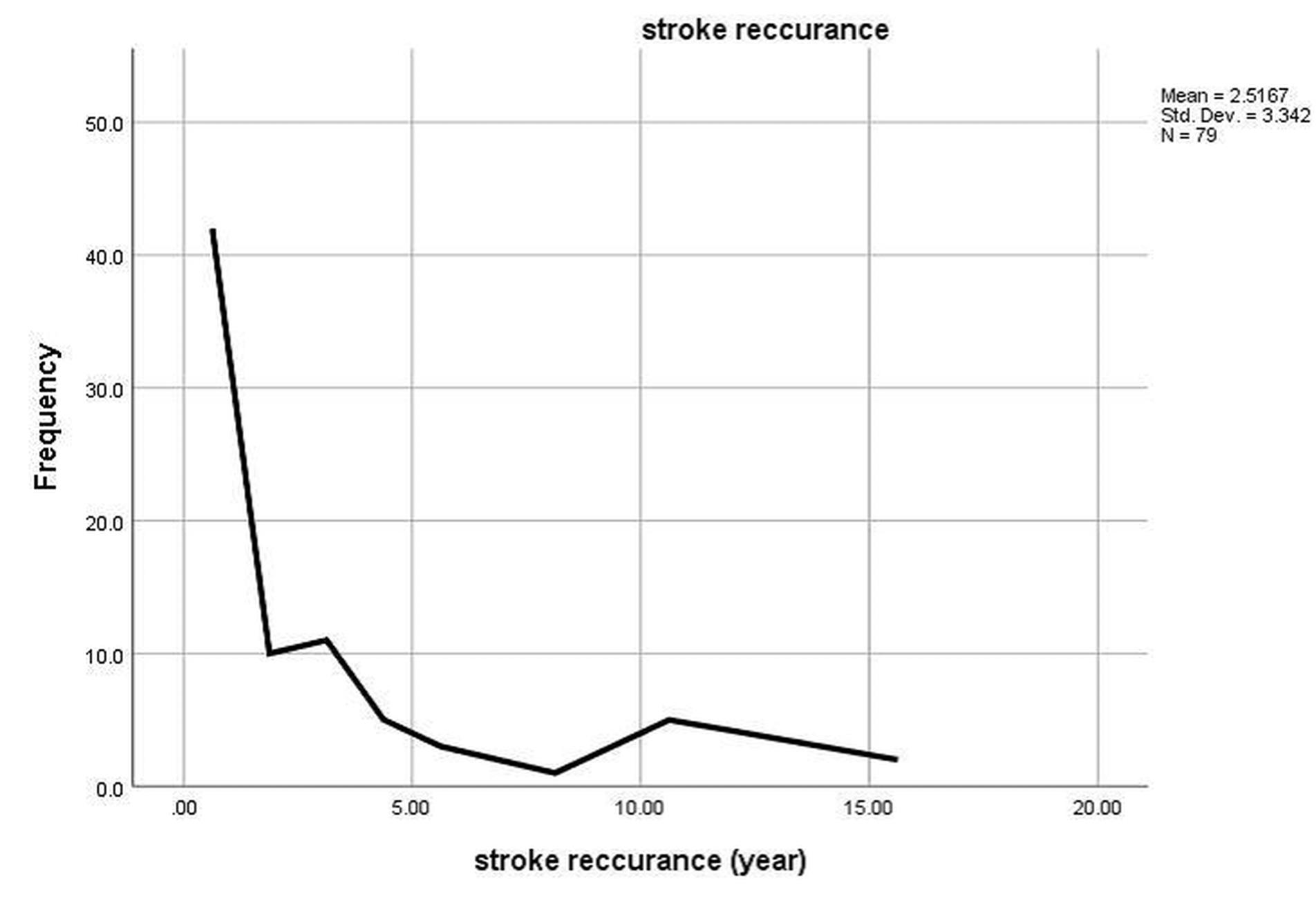
Figure 2.
Time interval of ischemic stroke recurrence in patients with ischemic stroke
.
Time interval of ischemic stroke recurrence in patients with ischemic stroke
Table 2.
Binary logistic regression analysis for prediction factors of recurrent ischemic events.
|
Variable
|
Risk ratio
|
95% Confidence intervals
|
| Hypertension |
0.76 |
0.17-3.45 |
| Diabetes mellitus |
0.45 |
0.14-1.48 |
| Heart diseases |
0.10 |
0.03-0.33 |
| Smoking |
1.13 |
0.24-5.47 |
| Age |
1.01 |
0.95-1.06 |
| Hyperlipidemia |
1.41 |
0.32-6.29 |
Discussion
In the present cohort study, we assessed clinical phenotypes and potential etiologies of stroke recurrence. Our findings showed no significant association between underlying diseases, smoking, and age with recurrence of ischemic stroke except for a history of heart diseases.
The risk of recurrent stroke most likely depends on the type of initial stroke. Mechanistically, various factors such as carotid stenosis, atherosclerosis, and atrial fibrillation are involved in the occurrence of recurrent form. However, early diagnosis of above-mentioned factors help us to better management of stroke recurrence.11 The importance of these diagnostic measures is to eliminate the etiology of the recurrent stroke and cerebrovascular diseases.12 Available evidence indicated that the rate of stroke recurrence in patients with intracranial or carotid atherosclerosis is higher than other causes.6 There are other reasons responsible for stroke recurrence which must be identified and managed promptly, including uncontrolled hypertension, atrial fibrillation, diabetes, hyperlipidemia, smoking, physical inactivity, and obstructive sleep apnea.6 In the first 12 months after the initial stroke, the risk of a recurrent stroke is between 8-12%, while, the risk of recurrent stroke reaches to 16.6% during five years.11 Noteworthy, mortality rate following second stroke is also higher than the initial stroke.9 The findings of a retrospective study indicated that the statistics about the risk of recurrent stroke is different in various countries, which can be due to differences in treatment and management methods, study methodology, and follow-up duration.13
Irie and colleagues included 368 stroke patients with a history of hypertension in the initial stroke hospitalization and second stroke attack during the follow-up period. In this study, a J-type relationship was identified between post-stroke diastolic blood pressure and stroke recurrence. Patients with measured diastolic blood pressure between 80 and 84 mmHg after stroke had a risk of recurrent stroke by 3.8%, which was significantly lower than other groups.14 In other population-based studies, blood pressure has been shown as an independent risk factor for ischemic stroke recurrence.15 In this regard, a recent systematic review and meta-analysis on risk factors of ischemic stroke recurrence showed that hypertension increased the risk of stroke recurrence by 1.67 time (odds ratio [OR]: 1.67, 95% CI: 1.45, 1.92, P < 0.00001).6 Similarly, the present study also showed that hypertension significantly increased the risk of ischemic stroke. However, our results showed no significant association between hypertension and recurrent ischemic stroke (RR: 0.76; 95% CI: 0.17-3.45). Additionally, in systolic blood pressure of 130 to 160 mm Hg, for every 10 mmHg increase in blood pressure, the probability of stroke recurrence increases by 28%.16 Therefore, controlled blood pressure greatly reduces the risk of cardiovascular diseases and could be considered one of the most important measures to prevent primary and recurrent strokes.11
In some studies, other unrelated factors have also been introduced as the cause of stroke recurrence, such as alcohol consumption, hyperlipidemia, and atrial fibrillation.17 The results showed that the history of heart diseases and arterial narrowing of large cerebral vessels is significantly related to the occurrence of recurrent stroke or transient ischemic attack one year after the initial stroke.11 Findings of the study conducted by Lai et al. showed that age, gender, history of hypertension, diabetes, and previous strokes were not related to ischemic stroke recurrence.18 According to University of Massachusetts Framingham studies, heart diseases were more likely to cause strokes. In addition, stroke occurs during ten years upon cardiovascular events such as myocardial infarction in the population that had no regular visits and follow-ups.19 In addition, an observational study showed that transient ischemic attack (OR: 2.98; 95% CI: 1.54-5.76), hypertension (OR: 1.96; 95% CI: 1.11-2.64), and atrial fibrillation (OR: 1.74; 95% CI 1.44-2.66) were significantly associated with recurrent ischemic stroke.20 Moreover, atrial fibrillation (OR: 1.88; 95% CI: 1.56, 2.25, P < 0.00001) and coronary heart disease (OR: 1.77, 95% CI: 1.31, 2.39, P = 0.0002) were significantly associated with ischemic stroke recurrence.6 In this line, our findings also showed a significant 90% lower risk of recurrent ischemic stroke in those without a history of heart diseases (RR: 0.10; 95% CI: 0.03-0.33).
Regarding age, a population-based study on 2874 patients with stroke showed that older age was associated with increased risk of recurrent stroke during ten years (P = 0.04), while significant results were not shown at one and five years follow-up.21 Our logistic regression analysis also showed no significant association between ischemic stroke recurrence and age during the period of study (RR: 1.01; 95% CI: 0.95-1.06).
We also found no significant association between diabetes mellitus (RR: 0.45; 95% CI: 0.14-1.48), smoking (RR: 1.13; 95% CI: 0.24-5.47), and ischemic stroke recurrence which could be due to the small sample size. Also, the results of a meta-analysis of 11 studies, including 14455 patients with initial stroke and 1545 patients with recurrent stroke showed that diabetes mellitus significantly increased the risk of recurrent stroke (OR: 1.50; 95% CI: 1.30-1.72, P < 0.00001), while smoking did not have a significant relationship with recurrent stroke (OR: 0.96; 95% CI: 0.80-1.15, P = 0.62).6 In parallel with these findings, another study also corroborated that diabetes mellitus was one of the significant predictors of stroke recurrence among other determinants.22,23
It has been also demonstrated that the history of hypercholesterolemia in people with atherosclerotic ischemic stroke was detected more than other types of ischemic stroke, and it predicts the possibility of intracranial atherosclerosis.24 Moreover, the results of the meta-analysis performed by Zheng et al revealed that dyslipidemia was not significantly associated with recurrent stroke (OR: 0.92; 95% CI: 0.67-1.27, P = 0.62).6 Similarly, we found no significant association between hyperlipidemia and ischemic stroke recurrence (RR: 1.41; 95% CI: 0.32-6.29). Therefore, further large-scale studies are needed to determine the relationship between stroke and hyperlipidemia.
Study Limitations
The present study has some limitations. First, we only included patients with ischemic stroke while other types and subtypes of the disease were not included. Second, due to the small sample size and being a single-center study, the findings cannot be generalized to other populations or other types of strokes. Third, during observational study, it is unable to determine a cause-effect relationship. Forth, the retrospective method of the research has limitations in terms of data collection, participant enrollment, and control group availability. Fifth, we only collected data regarding heart disease overall, while different types of cardiovascular diseases were not reported in the present study. Finally, due to the small sample size, we could not find a statistically significant association with various variables.
Study Highlights
What is current knowledge?
-
Cerebrovascular events, such as ischemic strokes, are among the most common causes of disability and the third leading cause of death in developed countries, with several risk factors contributing to stroke recurrence.
What is new here?
-
This study highlights a significant association between a history of heart disease and ischemic stroke recurrence, whereas other common conditions like hypertension, diabetes, smoking, and hyperlipidemia did not show a significant link to recurrent stroke in this cohort.
Conclusion
In this study, we found a reduced risk of stroke in patients without a history of heart diseases. Nevertheless, clinical evaluations and proper management of comorbidities in patients with stroke should be considered to reduce the risk of recurrent ischemic stroke. Therefore, further studies should evaluate the effects of controversial factors on ischemic stroke recurrence, using large-scale clinical studies.
Competing Interests
The authors declare that they have no conflicts of interests.
Consent for Publication
Not applicable.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due for they are personal data but are available from the corresponding author on reasonable request.
Ethical Approval
Written informed consent was obtained from all of the participants at the beginning of the study. The study protocol was approved by the ethics committee of Tabriz University of Medical Sciences, Tabriz, Iran (ethics code: IR.IAU.TABRIZ.REC.1400.039). All methods were performed in accordance with the national guidelines and regulations.
References
- Shah R, Wilkins E, Nichols M, Kelly P, El-Sadi F, Wright FL. Epidemiology report: trends in sex-specific cerebrovascular disease mortality in Europe based on WHO mortality data. Eur Heart J 2019; 40(9):755-64. doi: 10.1093/eurheartj/ehy378 [Crossref] [ Google Scholar]
- Coull AJ, Lovett JK, Rothwell PM. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. BMJ 2004; 328(7435):326. doi: 10.1136/bmj.37991.635266.44 [Crossref] [ Google Scholar]
- Kolmos M, Christoffersen L, Kruuse C. Recurrent ischemic stroke–a systematic review and meta-analysis. J Stroke Cerebrovasc Dis 2021; 30(8):105935. doi: 10.1016/j.jstrokecerebrovasdis.2021.105935 [Crossref] [ Google Scholar]
- Zhang J, Zhu P, Liu B, Yao Q, Yan K, Zheng Q. Time to recurrence after first-ever ischaemic stroke within 3 years and its risk factors in Chinese population: a prospective cohort study. BMJ Open 2019; 9(12):e032087. doi: 10.1136/bmjopen-2019-032087 [Crossref] [ Google Scholar]
- Petty GW, Brown RD Jr, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Survival and recurrence after first cerebral infarction: a population-based study in Rochester, Minnesota, 1975 through 1989. Neurology 1998; 50(1):208-16. doi: 10.1212/wnl.50.1.208 [Crossref] [ Google Scholar]
- Zheng S, Yao B. Impact of risk factors for recurrence after the first ischemic stroke in adults: a systematic review and meta-analysis. J Clin Neurosci 2019; 60:24-30. doi: 10.1016/j.jocn.2018.10.026 [Crossref] [ Google Scholar]
- Lin B, Zhang Z, Mei Y, Wang C, Xu H, Liu L. Cumulative risk of stroke recurrence over the last 10 years: a systematic review and meta-analysis. Neurol Sci 2021; 42(1):61-71. doi: 10.1007/s10072-020-04797-5 [Crossref] [ Google Scholar]
- Kwon HS, Lee D, Lee MH, Yu S, Lim JS, Yu KH. Post-stroke cognitive impairment as an independent predictor of ischemic stroke recurrence: PICASSO sub-study. J Neurol 2020; 267(3):688-93. doi: 10.1007/s00415-019-09630-4 [Crossref] [ Google Scholar]
- Khanevski AN, Bjerkreim AT, Novotny V, Naess H, Thomassen L, Logallo N. Recurrent ischemic stroke: incidence, predictors, and impact on mortality. Acta Neurol Scand 2019; 140(1):3-8. doi: 10.1111/ane.13093 [Crossref] [ Google Scholar]
- Kauw F, Takx RA, de Jong H, Velthuis BK, Kappelle LJ, Dankbaar JW. Clinical and imaging predictors of recurrent ischemic stroke: a systematic review and meta-analysis. Cerebrovasc Dis 2018; 45(5-6):279-87. doi: 10.1159/000490422 [Crossref] [ Google Scholar]
- Elkind MS. Outcomes after stroke: risk of recurrent ischemic stroke and other events. Am J Med 2009; 122(4 Suppl 2):S7-13. doi: 10.1016/j.amjmed.2009.02.005 [Crossref] [ Google Scholar]
- Demel SL, Kittner S, Ley SH, McDermott M, Rexrode KM. Stroke risk factors unique to women. Stroke 2018; 49(3):518-23. doi: 10.1161/strokeaha.117.018415 [Crossref] [ Google Scholar]
- Zhang C, Zhao X, Wang C, Liu L, Ding Y, Akbary F. Prediction factors of recurrent ischemic events in one year after minor stroke. PLoS One 2015; 10(3):e0120105. doi: 10.1371/journal.pone.0120105 [Crossref] [ Google Scholar]
- Irie K, Yamaguchi T, Minematsu K, Omae T. The J-curve phenomenon in stroke recurrence. Stroke 1993; 24(12):1844-9. doi: 10.1161/01.str.24.12.1844 [Crossref] [ Google Scholar]
- Sacco RL, Shi T, Zamanillo MC, Kargman DE. Predictors of mortality and recurrence after hospitalized cerebral infarction in an urban community: the Northern Manhattan Stroke Study. Neurology 1994; 44(4):626-34. doi: 10.1212/wnl.44.4.626 [Crossref] [ Google Scholar]
- Farrell B, Godwin J, Richards S, Warlow C. The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry 1991; 54(12):1044-54. doi: 10.1136/jnnp.54.12.1044 [Crossref] [ Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42(6):1206-52. doi: 10.1161/01.HYP.0000107251.49515.c2 [Crossref] [ Google Scholar]
- Lai SM, Alter M, Friday G, Sobel E. A multifactorial analysis of risk factors for recurrence of ischemic stroke. Stroke 1994; 25(5):958-62. doi: 10.1161/01.str.25.5.958 [Crossref] [ Google Scholar]
- Ois A, Gomis M, Rodríguez-Campello A, Cuadrado-Godia E, Jiménez-Conde J, Pont-Sunyer C. Factors associated with a high risk of recurrence in patients with transient ischemic attack or minor stroke. Stroke 2008; 39(6):1717-21. doi: 10.1161/strokeaha.107.505438 [Crossref] [ Google Scholar]
- Yalçın E, Yalçın M, Çelik Y, Ekuklu G. Risk factors for recurrent ischemic stroke in Turkey. Trakya Univ Tip Fak Derg 2008; 25(2):117-23. [ Google Scholar]
- Mohan KM, Crichton SL, Grieve AP, Rudd AG, Wolfe CD, Heuschmann PU. Frequency and predictors for the risk of stroke recurrence up to 10 years after stroke: the South London Stroke Register. J Neurol Neurosurg Psychiatry 2009; 80(9):1012-8. doi: 10.1136/jnnp.2008.170456 [Crossref] [ Google Scholar]
- Pennlert J, Eriksson M, Carlberg B, Wiklund PG. Long-term risk and predictors of recurrent stroke beyond the acute phase. Stroke 2014; 45(6):1839-41. doi: 10.1161/strokeaha.114.005060 [Crossref] [ Google Scholar]
- Hankey GJ, Jamrozik K, Broadhurst RJ, Forbes S, Burvill PW, Anderson CS. Long-term risk of first recurrent stroke in the Perth Community Stroke Study. Stroke 1998; 29(12):2491-500. doi: 10.1161/01.str.29.12.2491 [Crossref] [ Google Scholar]
- Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N. Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2008; 117(4):e25-146. doi: 10.1161/circulationaha.107.187998 [Crossref] [ Google Scholar]