J Res Clin Med. 12:6.
doi: 10.34172/jrcm.2024.33377
Case Report
Spontaneous intracerebral hemorrhage to reversible cerebral vasoconstriction syndrome: Case report
Tommy Alfandy Nazwar Conceptualization, Data curation, Supervision, Writing – original draft, 1, * 
Farhad Bal’afif Conceptualization, Funding acquisition, Investigation, Methodology, Validation, 1 
Donny Wisnu Wardhana Formal analysis, 1 
Akhmad Ferro Avisena Data curation, Formal analysis, Resources, Software, Visualization, 2
Mustofa Mustofa Project administration, Resources, Software, Visualization, Writing – original draft, 1
Author information:
1Division of Neurosurgery, Department of Surgery, Brawijaya University/Saiful Anwar Hospital Malang, East Java, Indonesia
2Department of Surgery, Brawijaya University/Saiful Anwar Hospital Malang, East Java, Indonesia
Abstract
Spontaneous intracerebral hemorrhage (sICH) is a common cause of morbidity and mortality in many countries. Hemorrhagic stroke occurs due to the internal hemorrhage inside the brain as a result of blood vessel rupture. Reversible cerebral vasoconstriction syndrome (RCVS) is multifocal arterial constriction and dilation in the cerebral vasculature and can cause subarachnoid hemorrhage and intracerebral hemorrhage (ICH). We present a case of diagnostic studies of sICH to RCVS in a patient with alcohol chronic consumption history.
Keywords: Intracranial hypertensive hemorrhages, Nonepileptic seizures, CT angiography, Reversible cerebral vasoconstriction syndrome
Copyright and License Information
© 2024 The Authors.
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
There was no grant for this research from any funding agency in the public, private, or not-for profit sectors.
Introduction
Cerebrovascular attack (CVA) or brain blood circulation disorder commonly known as a stroke is the third main cause of morbidity and mortality in many countries1 and in Indonesia in 2018 among people aged equal or more than 15 years old was predicted as many as 2 120 360 people.2 Hemorrhagic stroke contributes to 10%-20% of total stroke cases each year. The incident is approximately 12-15% cases per year, with much higher mortality than ischemic stroke.3 Intracerebral hemorrhage (ICH) is defined as intraparenchymal hemorrhage, referred to the spontaneous hemorrhage, which means a hemorrhage occurred without a known traumatic or structural disorder, like arteriovenous malformation (AVM), cerebral aneurism, or tumor.4
Reversible cerebral vasoconstriction syndrome (RCVS) is a group of conditions characterized by reversible multifocal narrowing of the cerebral arteries, in some cases, neurologic deficits caused by brain edema, stroke, or seizure.5 This condition might be caused by alcohol and/or narcotic consumption. MRI and CT scans are used in conventional diagnosis to investigate the symptoms of RCVS and ICH,6 the initial diagnosis and concentrated management are very important in ICH initial management. Other than a non-contrast CT scan, additional imaging modality can give important information about the ICH reason. The head computed tomography angiography (CTA) is conducted routinely on suspected spontaneous ICH patients due to the secondary etiology, RCVS, aneurism, AVM, tumor, or cerebral vena thrombosis. Dynamic angiographic anomalies support the idea that sudden changes in artery caliber could cause ischemia reperfusion damage, which would result in hemorrhages.5 This case is one of that which represents a rare case of severe intracranial hemorrhage with a normal Glasgow Coma Scale (GCS).
Case Presentation
A 30-year-old man was presented with the main complain of decreasing consciousness. The patient came with his family following five-time seizures each with duration of fewer than 5 minutes, with unknown interval among seizures, and unconsciousness during and after seizures. The patient had a seizure after drinking alcohol. The patient had come home with his consent from his previous hospital in Bali and had brought to Syaiful Anwar Hospital because there were no family members in Bali.
The main history of recent disease of patient was a stated whole-body seizure after drinking alcohol at the age of 18. After a day at Mangusada Hospital due to a history of malnutrition, the individual returned home with consent and received a prescription for medications, including domperidone (3 × 10 mg), tranexamic acid (3 × 500 mg), omeprazole (2 × 20 mg), and valproate (2 × 250 mg). Furthermore, patient denied the family history of hypertension, diabetes mellitus, heart disease and stroke. But he admits that he was a smoker, as well as narcotic consumption.
On physical examination general status, the patient is weak with Glasgow coma scale at 456, 123/84 mm Hg, with 70 times/minutes, respiration 20 times/minute, 36.7 °C and 98% on RA-SpO2. The patient was asked for head CTA. There was no abnormal cor and pulmo in normal boundary after X-ray chest-thorax examination (Figure 1). The ICH frontoparietal D vol 18 cc, with midline shift to left for 4 mm (Figure 2).

Figure 1.
Thorax examination on cor and pulmo boundary
.
Thorax examination on cor and pulmo boundary
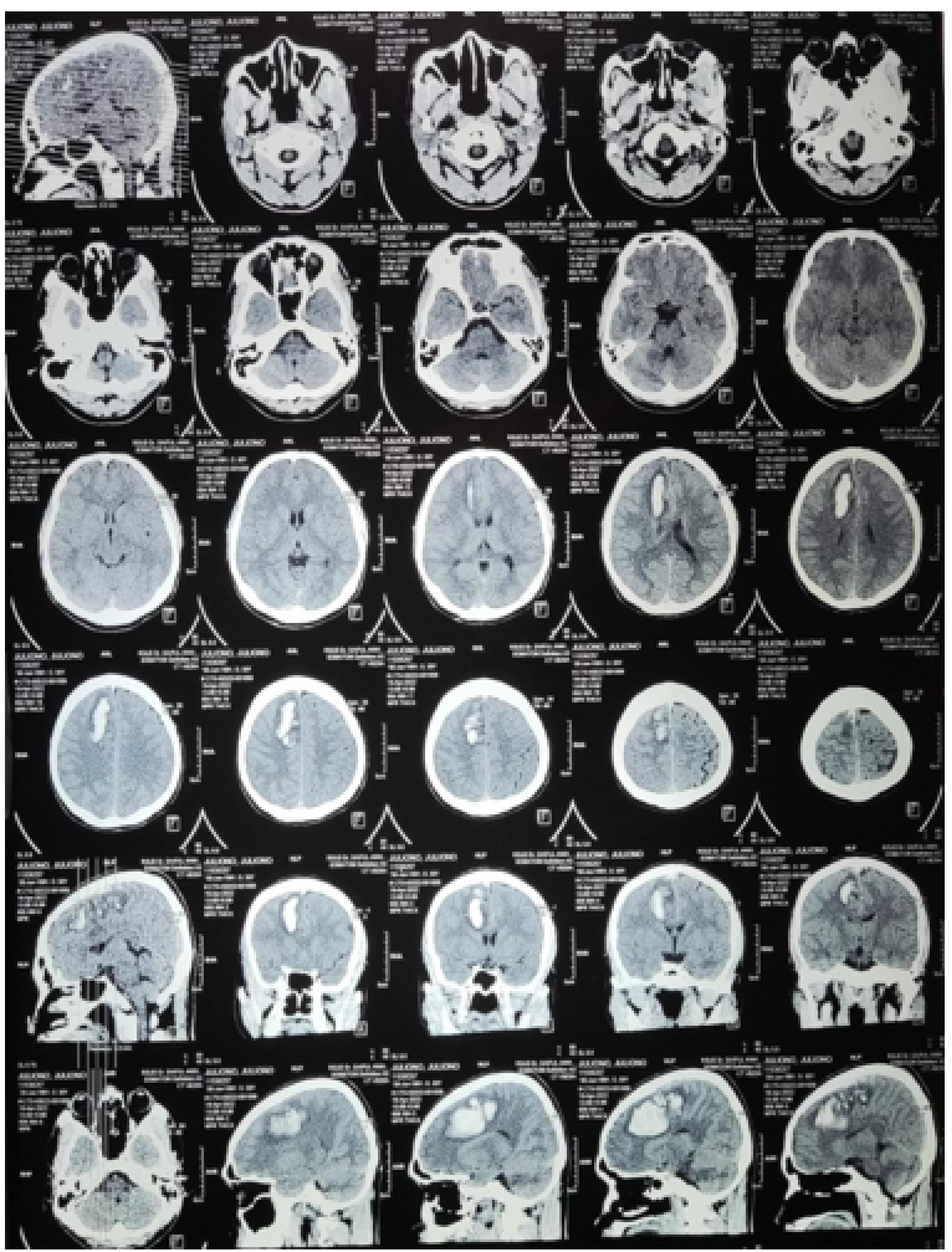
Figure 2.
Head CT scan examination ICH frontoparietal
.
Head CT scan examination ICH frontoparietal
The result of diagnosis stated that the patient had convulsion, CVA ICH frontoparietal D vol 18 cc and stage I hypertension. There was no aneurism or AVM (Figure 3). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee.
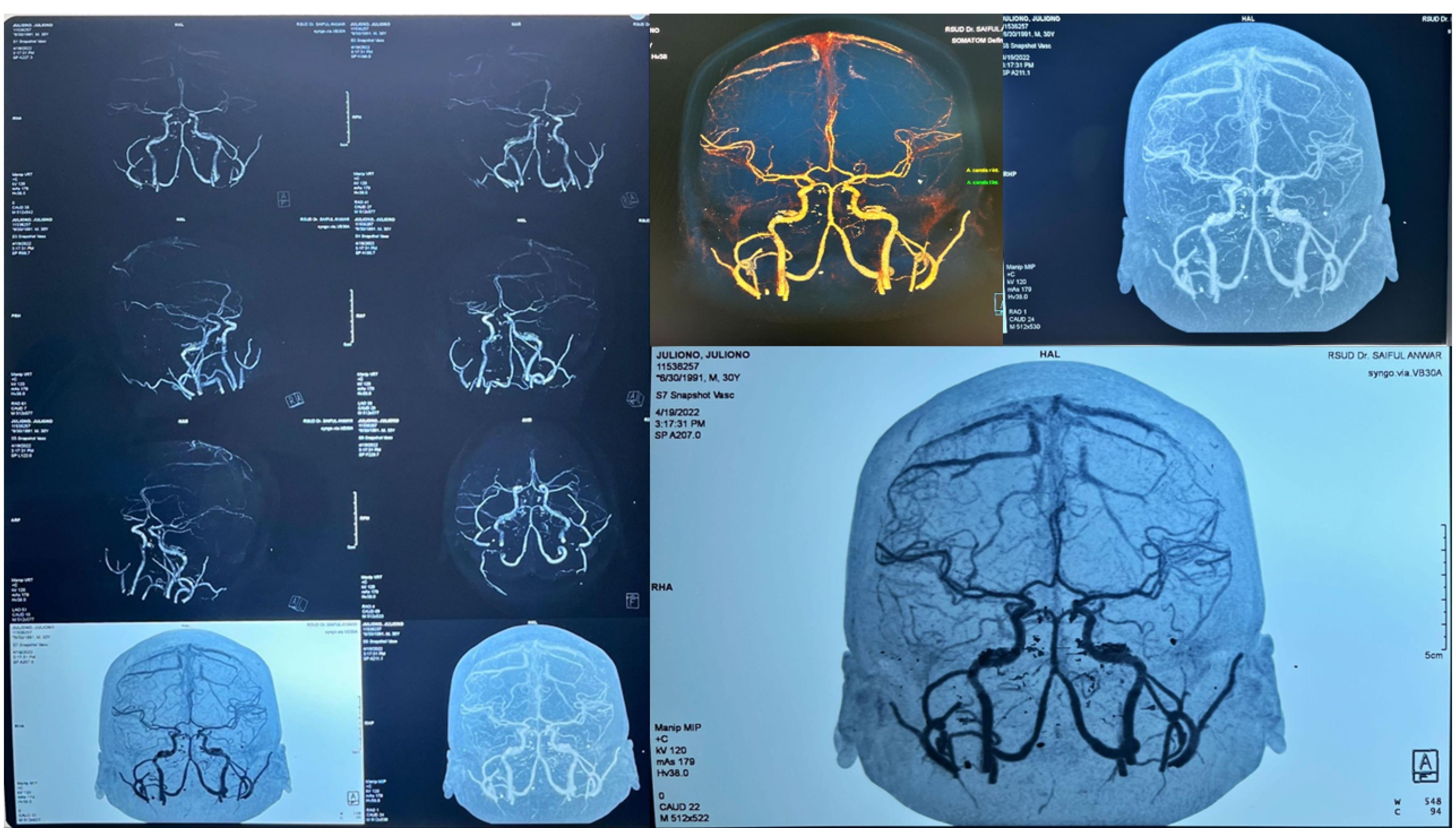
Figure 3.
Head CT angiography
.
Head CT angiography
Discussion
This patient was diagnosed with cerebrovascular accident ICH frontoparietal D vol 18 cc. It was obtained from anamnesis, physical examination, and supporting examination. The patient also admitted to using drugs and drinking alcohol in the past. A strong index of suspicion is necessary when diagnosing RCVS, a clinical entity and neurological emergency that is becoming more frequently identified but is still underrecognized. Although there are distinguishing characteristics in the history and on neuroimaging, overlapping findings with different illnesses might make a diagnosis challenging.7 We carried out additional research just utilizing magnetic resonance imaging data. The computerized tomography scan and digital subtraction cerebral angiograms, which are more accurate imaging modalities for distal vasoconstriction, were the only ones used in the novel angiographic analysis. Although there are several risk factors, so far, the main risk factor for spontaneous ICH is hypertension. Over time, the chronic stress at the blood vessel wall directs fragmentation, degeneration, and at the end the rupture of blood vessel leading to small blood penetration inside brain parenchyma. Hypertension hemorrhage tends to occur at a certain location, including structure inside ganglia basalis and thalamus, and pons, mesencephalon, and cerebellum.8
In this patient, several risk factors for stroke, such as excessive alcohol and narcotic consumption was discovered. Excessive alcohol consumption increases ICH risk through coagulopathy mechanism and systolic blood pressure increase. Drug abuse is also an important risk factor for spontaneous intracerebral hemorrhage (sICH). Amphetamine, cocaine, heroin, and ecstasy consumptions have been associated with sICH. Several mechanisms including blood pressure increase, heart arrhythmia followed by brain emboli, vasculitis, vasculopathy, and RCVS are responsible for the observed outcome.4
As first-line imaging, non-contrast computed tomography is so far the most common modality used to diagnose ICH and is very sensitive to detecting acute hemorrhage. After ICH diagnosis, CT angiography and MR imaging are very helpful to determine hemorrhage etiology and prognosis. CTA has advantages in defining artery vascular lesions and can help detect active hemorrhage that possibly causes hematoma expansion. It has been discovered that 96% of them are sensitive to detecting vascular malformation in ICH arrangement.9 Angiogram analysis showed more severe vasoconstriction in distal versus proximal segments in all lesion types. Spot sign is a hyperdense area indicating contrast media leak inside hematoma in the CTA that was conducted at ICH acute phase. Several studies have reported that the spot sign predicts the occurrence of hematoma expansion.10
Similar cases have been observed various researches. Hotta et al10 showed that 75% of 323 ICH patients had no sign of spot sign. Romero et al11 stated a very high negative predictive value (NPV) (0.98) for ICH to normal CTA patients that had no sign of spot sign. Another research conducted by Demchuk et al12 also showed an NPV value of 0.78. A very high NPV from CTA spot sign, especially the patient without IVH and antithrombotic therapy, shows that patient without spot sign is significantly at much lower risk for the next hematoma expansion romero.11 Meanwhile, hematoma expansion may occur in the patients without a spot sign, when there is a slow blood circulation from the artery and/or vein or intermittent hemorrhage from the artery Hotta.10
Looking back to the patient’s history of the previous disease, at age 18 the patient had experienced a seizure that was inducted by alcohol and then had recovered by itself. A possible hypothesis is that ICH triggered by RCVS can occur spontaneously and recover by itself. However, RCVS is often more associated with triggers, especially sympathomimetic drugs and/or other vasoactive substances. Suspected substances are including selective serotonin reuptake inhibitors (SSRIs), triptan, an ergot derivative, alpha sympathomimetic, and most of the forbidden drugs except the opium derivatives, and acute heavy drinking.13 Mathon et al13 stated that seven of 12 RCVS patients showed normal CTA at the beginning. Performing CTA again, several visible blood vessels constriction after seven days on average were detected (range: 3-18). This was also confirmed by brain digital subtraction angiography examination.
At many centers, CTA recently has substituted the digital subtraction angiography as an examination for hemorrhagic lesions and vascular. Mathon et al13 have stated formal MRI and DSA as the golden standard for ICH. Single CTA examination is considered as the reason for misdiagnosis or lack of diagnosis occur. Those explanations explain why there is no visible abnormal picture in this patient’s CTA. CTA examination on sICH is standard management. When a patient is clinically suspected of having sICH, head CTA scan is the standard diagnostic tool. However, it is limited by its single-case design, retrospective nature, the lack of a control group, and the absence of long-term follow-up data. While it offers valuable insights, these limitations in interpreting the findings stimulate further research in the field.
Conclusion
CTA procedures, whether contrast or not, need to be further improved to determine the degree of vasoconstriction in ICH. Alcohol and drug consumption have a strong role in the incidence of RCVS.
Acknowledgments
The researchers would like to express their gratitude to all the study participants from SMF Neurosurgery and Surgery Resident for their excellent participation.
Competing Interests
No conflicts of interest declared by the authors.
Ethical Approval
This study was approved by the Ethics Committee of Dr Saiful Anwar Hospital, Malang, Indonesia. Consent was explained and obtained from the subjects No 11536257. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
References
- Fernando SM, Qureshi D, Talarico R, Tanuseputro P, Dowlatshahi D, Sood MM. Intracerebral hemorrhage incidence, mortality, and association with oral anticoagulation use: a population study. Stroke 2021; 52(5):1673-81. doi: 10.1161/strokeaha.120.032550 [Crossref] [ Google Scholar]
- Riskesdas. Badan Penelitian dan Pengembangan Kesehatan Kementerian RI [Internet]. 2018. Available from: http://www.depkes.go.id/resources/download/infoterkini/materi_rakorpop_2018/Hasil%20Riskesdas%202018.pdf.
- Unnithan AK, Das JM, Mehta P. Hemorrhagic stroke. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022.
- Aguilar MI, Freeman WD. Spontaneous intracerebral hemorrhage. Semin Neurol 2010; 30(5):555-64. doi: 10.1055/s-0030-1268865 [Crossref] [ Google Scholar]
- Singhal AB. Reversible cerebral vasoconstriction syndromes: what the cardiologist should know. Curr Treat Options Cardiovasc Med 2014; 16(3):290. doi: 10.1007/s11936-013-0290-1 [Crossref] [ Google Scholar]
- Kim JY, Bae HJ. Spontaneous intracerebral hemorrhage: management. J Stroke 2017; 19(1):28-39. doi: 10.5853/jos.2016.01935 [Crossref] [ Google Scholar]
- Tan LH, Flower O. Reversible cerebral vasoconstriction syndrome: an important cause of acute severe headache. Emerg Med Int 2012; 2012:303152. doi: 10.1155/2012/303152 [Crossref] [ Google Scholar]
- Alerhand S, Lay C. Spontaneous intracerebral hemorrhage. Emerg Med Clin North Am 2017; 35(4):825-45. doi: 10.1016/j.emc.2017.07.002 [Crossref] [ Google Scholar]
- Kranz PG, Malinzak MD, Amrhein TJ. Approach to imaging in patients with spontaneous intracranial hemorrhage. Neuroimaging Clin N Am 2018; 28(3):353-74. doi: 10.1016/j.nic.2018.03.003 [Crossref] [ Google Scholar]
- Hotta K, Sorimachi T, Osada T, Baba T, Inoue G, Atsumi H. Risks and benefits of CT angiography in spontaneous intracerebral hemorrhage. Acta Neurochir (Wien) 2014; 156(5):911-7. doi: 10.1007/s00701-014-2019-7 [Crossref] [ Google Scholar]
- Romero JM, Hito R, Dejam A, Ballesteros LS, Cobos CJ, Liévano JO. Negative spot sign in primary intracerebral hemorrhage: potential impact in reducing imaging. Emerg Radiol 2017; 24(1):1-6. doi: 10.1007/s10140-016-1428-8 [Crossref] [ Google Scholar]
- Demchuk AM, Dowlatshahi D, Rodriguez-Luna D, Molina CA, Blas YS, Dzialowski I. Prediction of haematoma growth and outcome in patients with intracerebral haemorrhage using the CT-angiography spot sign (PREDICT): a prospective observational study. Lancet Neurol 2012; 11(4):307-14. doi: 10.1016/s1474-4422(12)70038-8 [Crossref] [ Google Scholar]
- Mathon B, Ducros A, Bresson D, Herbrecht A, Mirone G, Houdart E. Subarachnoid and intra-cerebral hemorrhage in young adults: rare and underdiagnosed. Rev Neurol (Paris) 2014; 170(2):110-8. doi: 10.1016/j.neurol.2013.07.032 [Crossref] [ Google Scholar]