J Res Clin Med. 12:28.
doi: 10.34172/jrcm.33349
Original Article
Multimorbidity raises the odds of decease in COVID-19 patients: An Iranian prospective study
Masood Faghih Dinevari Conceptualization, Project administration, Writing – review & editing, 1 
Mohammad Hossein Somi Conceptualization, Funding acquisition, Project administration, Writing – review & editing, 1
Leila Mokhtari Data curation, Investigation, Methodology, Project administration, Writing – review & editing, 2
Elham Sadeghi Majd Formal analysis, Writing – original draft, 3
Zeinab Nikniaz Conceptualization, Data curation, Formal analysis, Investigation, Resources, Software, Supervision, Validation, Writing – review & editing, 1, * 
Author information:
1Liver and Gastrointestinal Diseases Research Center, Tabriz University of medical sciences, Tabriz, Iran
2Imam Reza Hospital, Tabriz University of Medical Sciences, Tabriz, Iran
3Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Introduction:
The prevalence of noncommunicable diseases is high in Iran. We postulated that multimorbidity may affect the rate of mortality from COVID-19. So, we investigated the relationship between multimorbidity and COVID-19 mortality.
Methods:
We used medical reports for collecting clinical laboratory data of patients with COVID-19 in this prospective investigation. Moreover, we documented whether the patient had a known diagnosis of different comorbidities. The patients with more than one comorbidity were considered multimorbidity. The length of follow-up was till participants were discharged from the hospital or deceased. The main outcome was to evaluate the relationship between multimorbidity and death in COVID-19 hospitalized patients.
Results:
The present prospective study included 1842 patients with COVID-19 with a multimorbidity rate of 37.40%. About 24.6% of participants with more than four comorbidities died. However, this value was about 17% in participants with less than four comorbidities. The odds of mortality from COVID-19 were 53% greater in patients with diabetes. Also, the odds of death were 2.05 (1.21, 3.45) times greater in patients with comorbidities≥4.
Conclusion:
The results indicated a high rate of multimorbidity in patients with COVID-19 which is related to a higher death rate. So, in countries with higher multimorbidity rates such as Iran, it is necessary to design efficient approaches to alleviate the spread of COVID-19.
Keywords: Comorbidity, COVID-19, Hospitalization, Mortality, Multimorbidity
Copyright and License Information
© 2024 The Authors.
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
Liver and Gastrointestinal Diseases Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
Introduction
Coronavirus disease 2019 (COVID-19) is a contagious illness that was proclaimed as a pandemic in March 2020.1 The new disease had a high infection and mortality rate2 and among Asian countries, the infection rate in Iran was high.2
COVID-19 can vary from a mild disease with minor symptoms to serious pneumonia and multiorgan failure that cause death. Different comorbidities have been suggested as a factor contributing to severe disease and death from COVID-19.3 Several investigations have illustrated the higher chance of severe disease and pneumonia leading to intensive care, multi-organ failure, and death in patients with underlying comorbidities compared to patients without this situation. The list of common comorbidities in patients resulting in severe disease and hospitalization mainly includes hypertension, high blood sugar, heart disease, respiratory diseases, hepatic diseases, and anemia.3-8 However, little information is available regarding multimorbidity (patients with two or more underlying diseases) and COVID-19 intensity. In Italy, a higher mortality rate in patients with higher comorbidity scores was reported.9 In another study in Mexico, a significant positive relationship was reported between multimorbidity and death.10 Considering that the rate of noncommunicable diseases was high in Iran,11 we postulated that multimorbidity may affect the rate of death from COVID-19. Thus, we assessed the outcome of multimorbid patients infected with COVID-19 disease so that our results may help to identify the groups that are at high risk of severe illness and death and take preventative actions in this group of patients.
Materials and Methods
We used the East Azar COVID-19 Registry data for this prospective study. The criteria for registering patients in this registry were affirmative reverse transcription-polymerase chain reaction (RT-PCR) test results or lung imaging characteristics. Each patient provided informed consent.
Questionnaires were used to gather demographic and lifestyle-related characteristics. Medical reports were used for collecting clinical laboratory data. On admission, during Obtaining the medical history, the nurses asked the patients or primary next of kin, about the known diagnosis of cardiovascular-related diseases such as high blood pressure, heart attack, coronary revascularization, heart failure, high blood sugar, chronic kidney diseases, chronic pulmonary disease, higher body mass index than 30 kg/m2, history of cancers, and hepatic disease.
The participants were followed up until discharged from the hospital or deceased. All information was gathered by expert nurses, and quality was checked by one of the investigators.
The main outcome of this study was studying the relationship between multimorbid conditions and death in patients suffering from COVID-19.
Statistical analysis
We analyzed the collected data by SPSS version 25 (IBM Corporation, NY, USA). We applied the Kolmogorov-Smirnov test the normality of variables. The quantitative variable was stated as the mean (SD), and the qualitative data were shown as frequency (%). The between-group comparisons for constant data were done by independent t-test and for nominal and rank data by chi-square test, with Fisher’s exact test as needed. For examination of the relationship between comorbidities and multimorbidity with mortality from COVID-19, logistic regression was used. Demographic, lifestyle, and on-admission clinical factors that had a significant relationship in the univariate model were entered into the multivariate model. As a result, the odds ratios estimated by the logistic regression were adjusted for age, smoking, and dyspnea. The significant level was considered as a P value < 0.05.
Results
Totally 1842 patients with COVID-19 with a mean age of 63.07 ± 17.22 years were involved. In this investigation, 17.75% (327) of patients were deceased.
Comparison of the baseline characteristics
As presented in Table 1, in contrast to the survivors, the non-survivors were older (P < 0.001) and heavier smokers (P = 0.03). The two groups were almost comparable in terms of the frequency of comorbidities (P > 0.05). Regarding the presence of symptoms on admission, the frequency of hypoxia was significantly higher in non-survivors (52.59%) compared to survivors (30.16%) (P < 0.001).
Table 1.
The demographic characteristics of patients with COVID-19
|
Demographic variables
|
Total (n=1842)
|
Non-survivors (n=327)
|
Survivors (n=1515)
|
P
value
|
| Age (y), Mean ± SD |
63.07 ± 17.22 |
69.10 ± 14.51 |
61.76 ± 17.48 |
< 0.001* |
| Sex, Males, n (%) |
1019 (55.32) |
187 (57.18) |
832 (54.91) |
0.46** |
| Smoking, n (%) |
100 (5.42) |
23 (7.03) |
77 (5.08) |
0.03** |
| Comorbidities, n (%) |
|
|
|
|
| CVD |
843 (45.7) |
154 (47.1) |
689 (45.5) |
0.59** |
| Respiratory diseases |
229 (12.4) |
47 (14.3) |
182 (12.0) |
0.24** |
| Kidney diseases |
173 (9.4) |
32 (9.8) |
141 (9.3) |
0.78** |
| Diabetes |
423 (23) |
88 (26.9) |
335 (22.1) |
0.06** |
| Carcinoma |
81 (4.4) |
16 (4.9) |
65 (4.3) |
0.63** |
| Liver diseases |
37 (2.0) |
3 (0.9) |
34 (2.2) |
0.12** |
| Autoimmune diseases |
23 (1.2) |
1 (0.3) |
22 (1.5) |
0.09** |
| Mental diseases |
115 (6.2) |
26 (8) |
89 (5.9) |
0.15** |
| Musculoskeletal diseases |
42 (2.3) |
9 (2.8) |
33 (2.2) |
0.52** |
| Obesity |
397 |
62 (18.96) |
335 (22.11) |
0.35 |
| BMI (kg/m2), Mean ± SD |
27.54 ± 5.44 |
27.40 ± 5.10 |
27.57 ± 5.51 |
0.62* |
| Temperature (°C), Mean ± SD |
37.39 ± 13.72 |
37.1 ± 3.76 |
37.44 ± 4.91 |
0.65* |
| Hypoxia, n (%) |
629 (34.14) |
172 (52.59) |
457 (30.16) |
< 0.001** |
CVD, cardiovascular disease; HTN, hypertension; BMI, body mass index.
*P value of independent t-test; ** P value of chi-square test.
As can be seen in Table 2, 688 participants (37.40%) had multimorbidity. Cardiometabolic disorders predominantly accounted for the highest number of multimorbidity combinations observed: cardiovascular disease (CVD) and diabetes (287 patients), respiratory diseases and CVD (158 patients), CVD and kidney disease (124 patients), and diabetes and obesity (114 patients).
Table 2.
The most common co-occurring chronic diseases at baseline
|
|
CVD
|
Respiratory diseases
|
Diabetes
|
Obesity
|
Kidney diseases
|
Liver diseases
|
cancers
|
Autoimmune diseases
|
Nervous diseases
|
Muscular diseases
|
| Respiratory diseases |
158 |
|
|
|
|
|
|
|
|
|
| Diabetes |
287 |
68 |
|
|
|
|
|
|
|
|
| Obesity |
215 |
45 |
114 |
|
|
|
|
|
|
|
| Kidney diseases |
124 |
44 |
77 |
34 |
|
|
|
|
|
|
| Liver diseases |
19 |
8 |
1 |
14 |
7 |
|
|
|
|
|
| cancers |
40 |
17 |
24 |
11 |
11 |
3 |
|
|
|
|
| Autoimmune diseases |
14 |
5 |
8 |
10 |
2 |
1 |
2 |
|
|
|
| Mental diseases |
65 |
24 |
1 |
25 |
10 |
6 |
9 |
1 |
|
|
| Musculoskeletal diseases |
27 |
12 |
4 |
15 |
7 |
5 |
5 |
4 |
12 |
|
| HIV |
1 |
1 |
0 |
0 |
0 |
0 |
0 |
0 |
1 |
0 |
As depicted in Figure 1, the number of multi-morbidities was higher in older patients (P < 0.05).
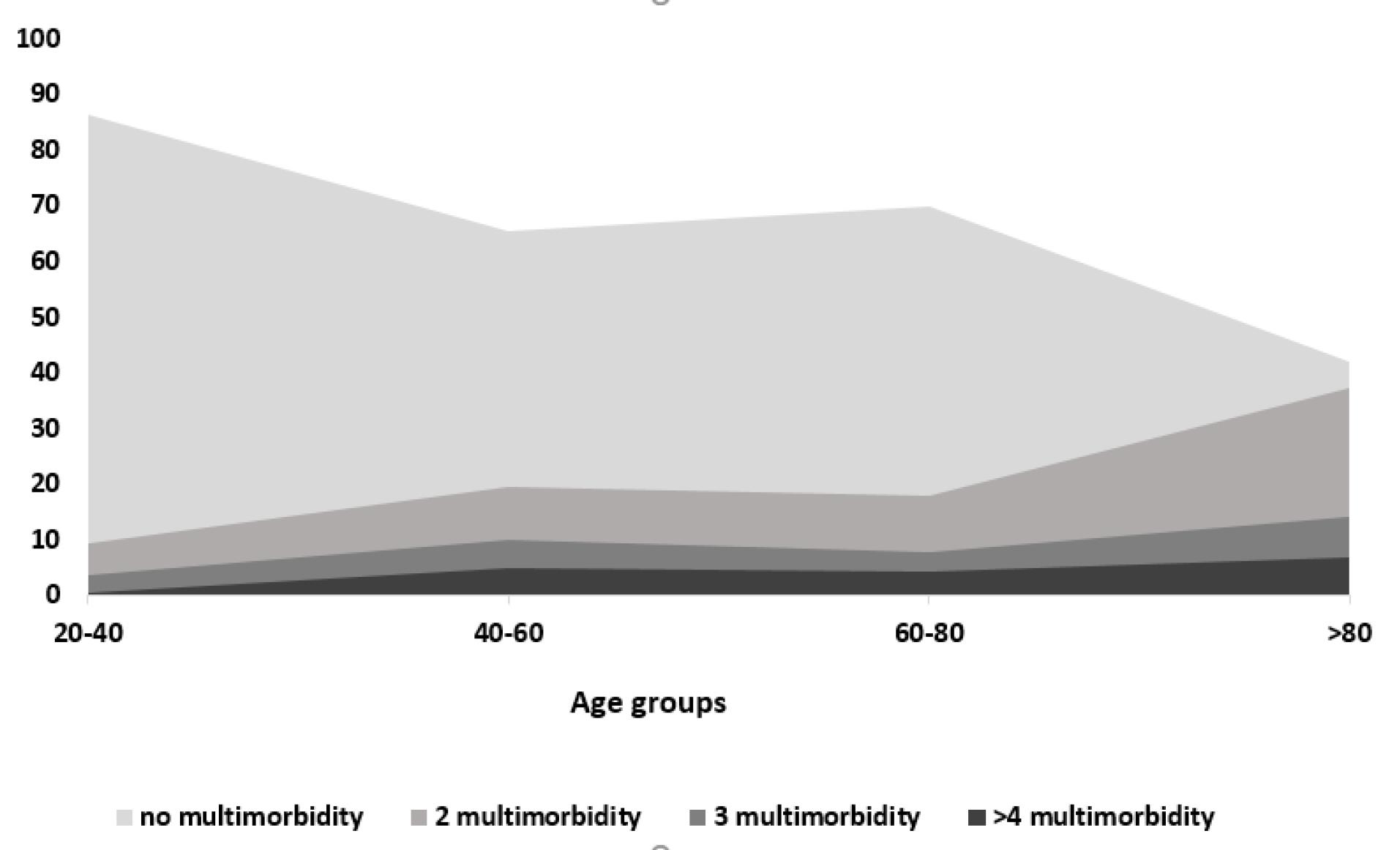
Figure 1.
The multimorbidity status according to age
.
The multimorbidity status according to age
As shown in Figure 2, 24.6% of participants with more than four comorbidities died. However, this value was approximately 17% in participants with less than four comorbidities.
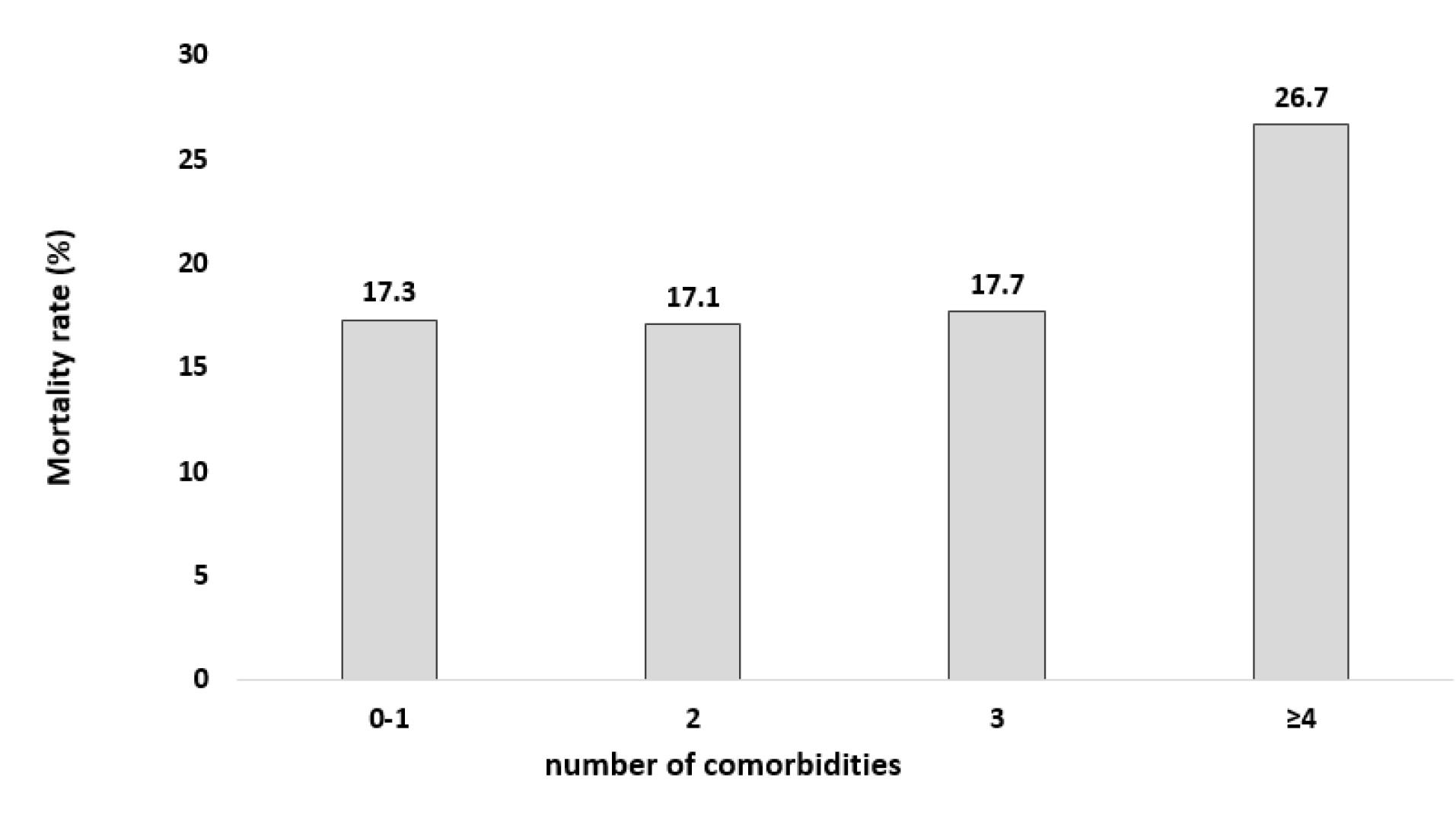
Figure 2.
The rate of mortality in patients with COVID-19 stratified by number of co-morbidities
.
The rate of mortality in patients with COVID-19 stratified by number of co-morbidities
Relationship between comorbidities and mortality from COVID-19
Table 3 presents the association between comorbidities and death during attendance in the hospital in patients with COVID-19. The odds of death were 53% greater in patients with diabetes. Additionally, patients with comorbidities ≥ 4 had less chance of survival from COVID-19 (OR: 2.05; 95% CI: 1.21, 3.45). However, no significant correlation was observed between other comorbidities and death in this study.
Table 3.
The logistic regression analysis of comorbidities and death during hospitalization in patients with COVID-19
|
Variables
|
Multivariate model*
|
|
Odds ratio
|
CI
|
P
value
|
| CVD |
1.07 |
0.94-2.59 |
0.07 |
| Respiratory daises |
1.32 |
0.91-1.91 |
0.14 |
| Kidney diseases |
1.11 |
0.72-1.73 |
0.61 |
| Cancers |
1.31 |
0.71-2.42 |
0.38 |
| Autoimmune diseases |
0.35 |
0.04-2.67 |
0.31 |
| Diabetes |
1.53 |
1.13-2.06 |
0.005 |
| Liver diseases |
0.53 |
0.16-1.79 |
0.31 |
| Mental diseases |
1.54 |
0.94-2.52 |
0.08 |
| Musculoskeletal diseases |
1.32 |
0.59-2.99 |
0.49 |
| Multimorbidity |
|
|
|
| 0-1 |
Ref |
Ref |
Ref |
| 2 |
1.15 |
0.83-1.60 |
0.37 |
| 3 |
1.12 |
0.72-1.74 |
0.60 |
| > 4 |
2.05 |
1.21-3.45 |
0.007 |
CVD, cardiovascular disease; HTN, hypertension; BMI, body mass index.
Dependent variable: Death.
Adjusted for age, smoking and hypoxia.
Discussion
Previously, different investigations showed that comorbidities increase mortality and disease severity in patients with COVID-19.3,6 Nevertheless, some researches have focused on the relationship between multimorbid conditions and COVID-19 outcomes. The current study result showed that 37.4% of patients with COVID-19 had multimorbidity in Iran. This value is higher than the rate of multimorbidity in Mexico (19.1%).10 However, it is lower than the reported multimorbidity rate in the UK (43.1%)12 and the United States (88%).3 The differences in the multimorbidity rate between the studies may be due to the dissimilarities in the age groups of participants. As reported in the present study and a previous study, the rate of multimorbidity increases with age.9 In addition, differences in multimorbidity prevalence in the community could also affect the frequency of multimorbidity in patients with COVID-19. In addition, dissimilarities in multimorbidity definition in various studies could also be considered another justification for differences in the multimorbidity rate in various studies.
In line with previous studies, the most prevalent multi-morbidities were related to cardiometabolic conditions.6 According to the report of a systematic review, in different studies, high blood pressure, high normal weight, and diabetes were reported as the most prevalent comorbidities in hospitalized COVID-19 patients.13 This may be related to impaired immune function and inflammatory response and the type of medications used by patients. For example, most patients with cardiometabolic conditions use angiotensin-converting enzyme (ACE) inhibitors, which increase the expression of the ACE2 receptor, allowing the entrance of SARS-CoV-2 to different cells.14
Our results indicated higher chance of death in patients with multi-morbidities ≥ 4. Our result was in agreement with the earlier studies’ findings. Iaccarino et al reported a higher death rate in patients with COVID-19 who had higher comorbidity scores.9 In another study in Mexico, a significant positive relationship was reported between multimorbidity and death.10 Although the higher mortality rate due to multimorbidity could partly be attributed to the higher age,15 in our study, the relationship between multimorbidity and death was still significant even after adjusting the results for age. Therefore, the observed association between multimorbidity and death may be partly due to the higher psychological stress in patients with multimorbidity.16 On the other hand, COVID-19 is also associated with higher psychological stress.17,18 Studies have shown that psychological stress is related to a higher mortality rate.19 In patients with COVID-19, the presence of multimorbidity influences physical and psychological health, mainly in developing countries.20 This influence on the response to treatment in these patients.10
Higher inflammatory factors in patients with multimorbidity is another mechanism that may support our findings.21 Higher rates of mortality in patients with COVID-19 who had higher inflammatory cytokine levels have been reported.22,23
The present study suffers from some limitations, including using single-center data that bring into question the generalizability. However, the center we collected our data is the focal point for COVID-19 in our region. Besides, our participants were patients who attended the hospital, and we cannot comment on the associations between multimorbidity and mortality in the community.
Study Highlights
What is current knowledge?
-
The list of common comorbidities in patients resulting in severe disease and hospitalization in patients with COVID-19 is available
-
They mainly includes hypertension, high blood sugar, heart disease, respiratory diseases, hepatic diseases, and anemia
-
Little information is available regarding multimorbidity and COVID-19 intensity
What is new here?
-
The multimorbidity rate in patients with COVID-19 was 37.40%.
-
About 24.6% of participants with more than four comorbidities died.
-
The odds of mortality from COVID-19 were 53% greater in patients with diabetes.
-
The odds of death were significantly higher in patients with comorbidities≥4
Conclusion
In conclusion, our finding showed the high rate of multimorbidity in patients with COVID-19 which is also associated with a higher mortality rate in these patients. Therefore, in countries with higher multimorbidity rates, such as Iran, it is essential to design efficient approaches to alleviate the spread of COVID-19 within these specific groups to diminish the influence of COVID-19 on healthcare organizations.
Competing Interests
The authors have no conflicts of interest to declare.
Ethical Approval
The research ethics committee of Tabriz University of Medical Sciences, Iran approved the study (code: IR.TBZMED.REC.1398.1274) and a written informed consent was obtained from all patients.
References
- Esakandari H, Nabi-Afjadi M, Fakkari-Afjadi J, Farahmandian N, Miresmaeili SM, Bahreini E. A comprehensive review of COVID-19 characteristics. Biol Proced Online 2020; 22:19. doi: 10.1186/s12575-020-00128-2 [Crossref] [ Google Scholar]
- Worldometer. Coronavirus Update. Available from: https://www.worldometers.info/coronavirus/. Accessed September 19, 2020.
- Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020; 323(20):2052-9. doi: 10.1001/jama.2020.6775 [Crossref] [ Google Scholar]
- Nikniaz Z, Faghih Dinevari M, Mokhtari L. Association of cardiovascular disease, respiratory diseases, and diabetes treatment with COVID-19 mortality in hospitalized patients. Int J Drug Res Clin 2023; 1(1):e21. doi: 10.34172/ijdrc.2023.e21 [Crossref] [ Google Scholar]
- Faghih Dinevari M, Somi MH, Sadeghi Majd E, Fattahzadeh A, Nikniaz Z. Elevated liver aminotransferases level and COVID-19 prognosis in hospitalized patients: a prospective study from Iran. Middle East J Dig Dis 2022; 14(1):64-9. doi: 10.34172/mejdd.2022.257 [Crossref] [ Google Scholar]
- Chudasama YV, Gillies CL, Appiah K, Zaccardi F, Razieh C, Davies MJ. Multimorbidity and SARS-CoV-2 infection in UK Biobank. Diabetes Metab Syndr 2020; 14(5):775-6. doi: 10.1016/j.dsx.2020.06.003 [Crossref] [ Google Scholar]
- Faghih Dinevari M, Somi MH, Sadeghi Majd E, Abbasalizad Farhangi M, Nikniaz Z. Anemia predicts poor outcomes of COVID-19 in hospitalized patients: a prospective study in Iran. BMC Infect Dis 2021; 21(1):170. doi: 10.1186/s12879-021-05868-4 [Crossref] [ Google Scholar]
- Nikniaz Z, Somi MH, Faghih Dinevari M, Taghizadieh A, Mokhtari L. Diabesity associates with poor COVID-19 outcomes among hospitalized patients. J Obes Metab Syndr 2021; 30(2):149-54. doi: 10.7570/jomes20121 [Crossref] [ Google Scholar]
- Iaccarino G, Grassi G, Borghi C, Ferri C, Salvetti M, Volpe M. Age and multimorbidity predict death among COVID-19 patients: results of the SARS-RAS study of the Italian Society of Hypertension. Hypertension 2020; 76(2):366-72. doi: 10.1161/hypertensionaha.120.15324 [Crossref] [ Google Scholar]
- Hernández-Vásquez A, Azañedo D, Vargas-Fernández R, Bendezu-Quispe G. Association of comorbidities with pneumonia and death among COVID-19 patients in Mexico: a nationwide cross-sectional study. J Prev Med Public Health 2020; 53(4):211-9. doi: 10.3961/jpmph.20.186 [Crossref] [ Google Scholar]
- Esteghamati A, Meysamie A, Khalilzadeh O, Rashidi A, Haghazali M, Asgari F. Third national Surveillance of Risk Factors of Non-Communicable Diseases (SuRFNCD-2007) in Iran: methods and results on prevalence of diabetes, hypertension, obesity, central obesity, and dyslipidemia. BMC Public Health 2009; 9:167. doi: 10.1186/1471-2458-9-167 [Crossref] [ Google Scholar]
- Woolford SJ, D’Angelo S, Curtis EM, Parsons CM, Ward KA, Dennison EM, et al. COVID-19 and associations with frailty and multimorbidity: a prospective analysis of UK Biobank participants. medRxiv [Preprint]. June 11, 2020. Available from: https://www.medrxiv.org/content/10.1101/2020.06.09.20126292v1.full.
- Baradaran A, Ebrahimzadeh MH, Baradaran A, Kachooei AR. Prevalence of comorbidities in COVID-19 patients: a systematic review and meta-analysis. Arch Bone Jt Surg 2020; 8(Suppl 1):247-55. doi: 10.22038/abjs.2020.47754.2346 [Crossref] [ Google Scholar]
- de Lucena TMC, da Silva Santos AF, de Lima BR, de Albuquerque Borborema ME, de Azevêdo Silva J. Mechanism of inflammatory response in associated comorbidities in COVID-19. Diabetes Metab Syndr 2020; 14(4):597-600. doi: 10.1016/j.dsx.2020.05.025 [Crossref] [ Google Scholar]
- Violan C, Foguet-Boreu Q, Flores-Mateo G, Salisbury C, Blom J, Freitag M. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS One 2014; 9(7):e102149. doi: 10.1371/journal.pone.0102149 [Crossref] [ Google Scholar]
- Prior A, Fenger-Grøn M, Larsen KK, Larsen FB, Robinson KM, Nielsen MG. The association between perceived stress and mortality among people with multimorbidity: a prospective population-based cohort study. Am J Epidemiol 2016; 184(3):199-210. doi: 10.1093/aje/kwv324 [Crossref] [ Google Scholar]
- Kempuraj D, Selvakumar GP, Ahmed ME, Raikwar SP, Thangavel R, Khan A. COVID-19, mast cells, cytokine storm, psychological stress, and neuroinflammation. Neuroscientist 2020; 26(5-6):402-14. doi: 10.1177/1073858420941476 [Crossref] [ Google Scholar]
- Willadsen TG, Siersma V, Nicolaisdóttir DR, Køster-Rasmussen R, Jarbøl DE, Reventlow S. Multimorbidity and mortality: a 15-year longitudinal registry-based nationwide Danish population study. J Comorb 2018; 8(1):2235042x18804063. doi: 10.1177/2235042x18804063 [Crossref] [ Google Scholar]
- De Silva RA. Psychological stress and sudden cardiac death. In: Schmidt TH, Dembroski TM, Blümchen G, eds. Biological and Psychological Factors in Cardiovascular Disease. Berlin, Heidelberg: Springer; 1986. p. 155-83. 10.1007/978-3-642-71234-0_12.
- Arokiasamy P, Uttamacharya U, Jain K, Biritwum RB, Yawson AE, Wu F. The impact of multimorbidity on adult physical and mental health in low- and middle-income countries: what does the study on global ageing and adult health (SAGE) reveal?. BMC Med 2015; 13:178. doi: 10.1186/s12916-015-0402-8 [Crossref] [ Google Scholar]
- Friedman EM, Christ SL, Mroczek DK. Inflammation partially mediates the association of multimorbidity and functional limitations in a national sample of middle-aged and older adults: the MIDUS study. J Aging Health 2015; 27(5):843-63. doi: 10.1177/0898264315569453 [Crossref] [ Google Scholar]
- Foroughi P, Varshochi M, Hassanpour M, Amini B, Nikniaz Z, Amini H. The predictive role of age and the systemic inflammation indexes on ICU admission and mortality in patients with COVID-19. Int J Aging 2023; 1(1):e10. doi: 10.34172/ija.2023.e10 [Crossref] [ Google Scholar]
- Del Valle DM, Kim-Schulze S, Huang HH, Beckmann ND, Nirenberg S, Wang B. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat Med 2020; 26(10):1636-43. doi: 10.1038/s41591-020-1051-9 [Crossref] [ Google Scholar]