J Res Clin Med. 12:19.
doi: 10.34172/jrcm.32267
Case Report
Large bilateral non-functional adrenal myelolipomas: A rare case report
Ebrahim Farashi Data curation, Investigation, Visualization, Writing – original draft, 1, 2 
Monireh Halimi Data curation, Visualization, 3 
Seyed Ziaeddin Rasihashemi Conceptualization, Methodology, Project administration, Supervision, Validation, Writing – review & editing, 1, * 
Author information:
1Department of Cardiothoracic Surgery, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
2Department of Surgery, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
3Department of Pathology, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Myelolipomas are rare, benign, and non-functional neuroendocrine tumors that are usually discovered incidentally. The widespread use of imaging modalities has increased the detection of incidental tumors over the last decades. Most myelolipomas are small, unilateral, and asymptomatic. Occasionally, tumors grow over time and become symptomatic due to the mass effect on adjacent structures. As a therapeutic approach, surgery is known as the standard treatment for symptomatic or large lesions. We report a patient presented with persisted abdominal pain which had been initiated two months ago. Ultrasonography examination showed large, bilateral, and well-defined hyperechoic lesions without calcification in both adrenal glands. Tumors were non-functional with hormone secretion-wise. After laparoscopic resection, on the macroscopic examination, two adrenal lesions with 60×50×40 mm and 35×30×10 mm size, respectively, were observed. The subsequent microscopic assessment also confirmed the diagnosis of bilateral adrenal myelolipomas.
Keywords: Adrenalectomy, Endocrinology, Myelolipoma, Neoplasms
Copyright and License Information
© 2024 The Authors.
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
Not applicable.
Introduction
Adrenal myelolipomas are rare, benign, and nonfunctional neuroendocrine tumors that are usually discovered incidentally. The widespread use of imaging modalities has increased the detection of incidental tumors over the last decades.1-3 In general, 9% of the population has adrenal masses. Adrenal myelolipomas comprise about 3%–5% of all primary tumors in the adrenal glands,4,5 which is more common among people aged between 50-70 years old. The incidence in both genders is nearly equal.6 Myelolipomas are adrenal or extra-adrenal masses composed of adipose and hematopoietic tissues.7 Most myelolipomas are small, unilateral, and asymptomatic. These tumors grow over time and become symptomatic due to pressure on adjacent viscera.4 Surgery is defined as the standard therapeutic approach for either symptomatic or large asymptomatic lesions.8 The aim of this case report is to define the diagnosis and appropriate approach of a non-functional myelolipoma in a patient. Additional information about rare adrenal myelolipomas occurrence and the representing of similar cases is crucial for clinicians to establish a consensus and prevent misdiagnosis and unsuitable management.
Case Presentation
A 51-year-old female was referred to our clinic with a complaint of pain or discomfort in the abdomen that persisted for two months. The patient had no history of previous surgeries or known medical conditions. An evaluation of her vital signs, including blood pressure and heart rate, showed no significant alterations. Physical examination and cardiovascular assessments were also normal. Ultrasound examinations demonstrated a well-defined hyperechoic lesion measuring 62 × 68 mm adjacent to the upper pole of the left kidney and a similar lesion of 42 × 32 mm adjacent to the upper pole of the right kidney, indicating adrenal fatty masses. Chest x-ray showed no detectable abnormalities. The laboratory results of the patient’s blood count, biochemistry profile, and urine biochemistry markers were in the reference range. Moreover, evaluations of thyroid function showed no apparent abnormalities (Table 1). Complementary imaging assessment of the abdomen was performed using an intravenous contrast-enhanced computed tomography (CT) scan. The CT detected a well-defined 77 × 63 mm hyperdense lesion showing low attenuation [-71 Hounsfield unit (HU)], containing adipose and vascular tissue without calcification. In addition, a 55 × 40 mm fat-containing solid lesion with a thin capsule and no enhancement on the right adrenal gland was detected (Figure 1).
Table 1.
Endocrine function evaluation
|
Tests
|
Unit
|
Reference range
|
Results
|
| WBC |
µL |
4000-14 300 |
6300 |
| Thyroid-stimulating hormone (TSH) |
μIU/mL |
0.4–4.2 |
0.848 |
| DHEA-SO4 |
µg/dL |
80-560 |
130.0 |
| Urine cortisol |
µg/24 h |
4.3–176 |
54.4 |
| Serum creatinine |
mg/dL |
0.6-1.3 |
0.7 |
| Urine creatinine |
g/24 h |
0.8–1.8 |
1.56 |
| Plasma renin activity in the supine position |
ng/mL/h |
0.06–4.69 |
1.03 |
| Aldosterone in the supine position |
ng/dL |
3.7–31.0 |
4.8 |
| Plasma free metanephrines |
pg/mL |
12–60 |
16.80 |
| 24 hr urine metanephrines |
mcg/24 h |
25–312 |
38.6 |
| Plasma aldosterone/renin ratio |
- |
2–17 |
4.66 |
| 24 hr urine normetanephrines |
mcg/24 h |
< 600 |
90.7 |
| Free thyroxine (FT4) |
Ng/dL |
0.8–1.8 (21-54 Y) |
0.869 |
| Serum cortisol |
µg/dL |
8 AM: 5–23, 4 PM: 3–13 |
5.61 |
| C-Reactive Protein |
mg/L |
8-10 ˃ |
Negative |
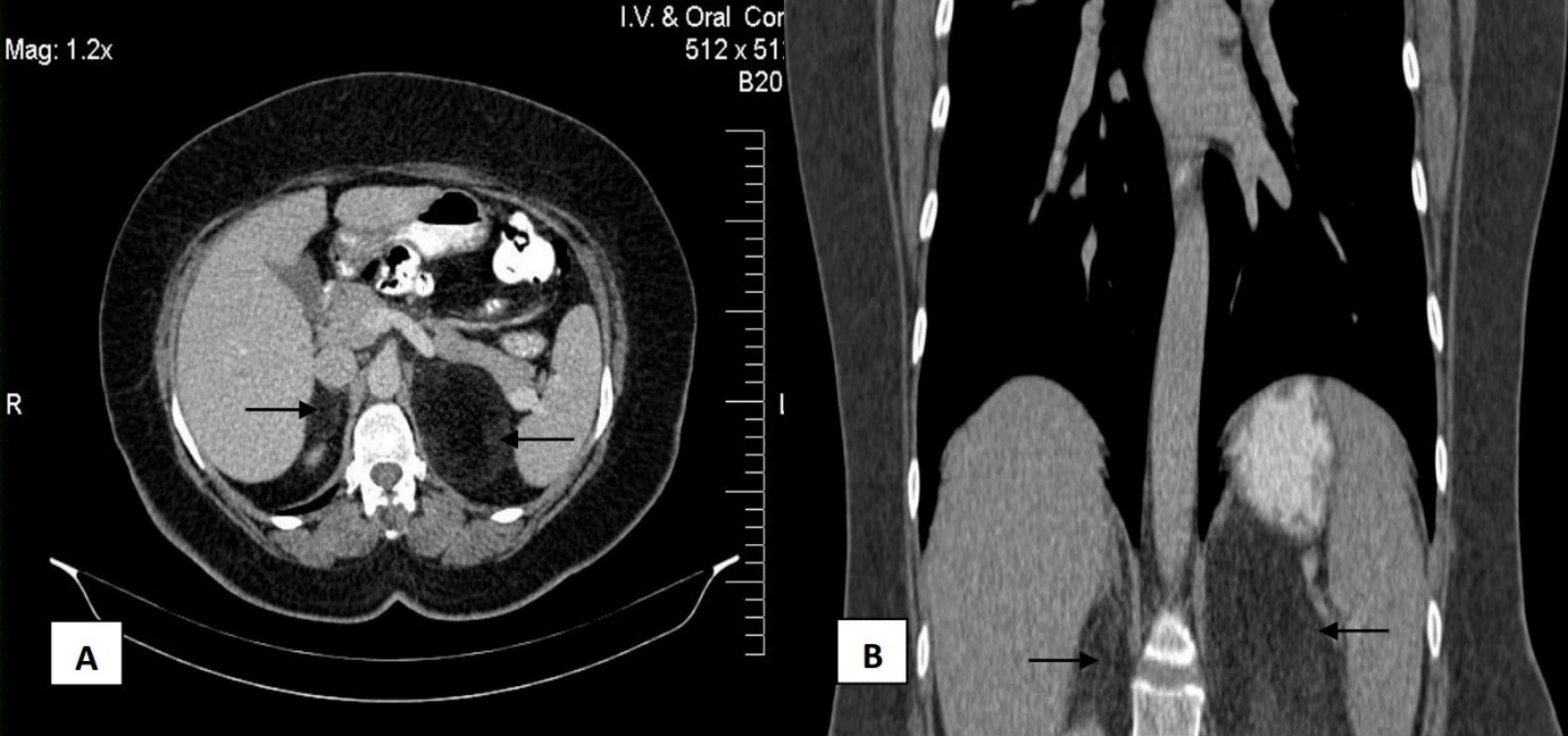
Figure 1.
CT scan. (A) The cross-sectional CT scan shows bilateral lesions of the surrounded left and right renal with 77 × 63 mm and 55 × 40 mm, respectively. (B) The coronal-sectional CT scan
.
CT scan. (A) The cross-sectional CT scan shows bilateral lesions of the surrounded left and right renal with 77 × 63 mm and 55 × 40 mm, respectively. (B) The coronal-sectional CT scan
Considering the patient’s symptoms and para-clinic findings, a bilateral laparoscopic adrenalectomy was performed. The patient was placed in the right lateral decubitus and reversed to the Trendelenburg position. First, resection of the left adrenal mass was performed due to its larger size. Three ports were inserted into the left subcostal region. The splenic flexure of the colon, the line of Toldt, and the splenocolic ligament were incised. The left renal vein and adrenal gland were exposed by dissecting the avascular plane between the anterior aspect of the Gerota’s fascia and the posterior surface of the pancreas.
After detecting the renal vein, the adrenal vein and the left suprarenal and adrenal branches of the phrenic artery were ligated. The left adrenal gland was carefully dissected from the diaphragm. Finally, the adrenal gland was placed in a retrieval bag and removed through the largest port (Figure 2). For resection of the adrenal mass on the right side, the patient was positioned in the left lateral decubitus, four ports were placed, and the above-mentioned steps were repeated. Then, the right triangular ligament of the liver was isolated, and the liver was retracted in the cephalic direction using a cobra liver retractor inserted through the epigastric trocar. The inferior vena cava (IVC) was identified as a hallmark. When the adrenal vein was exposed through a peritoneal incision in the lateral part of the IVC, it was ligated and incised. The adrenal mass was released with the right adrenal gland and dissected. After removing the mass, a Jackson Pratt drain was inserted into the operation site to drain fluids (Figure 2). The left mass had a size of 60 × 50 × 40 mm (Figure 3). The right mass (35 × 30 × 10 mm) with a yellowish homogeneous composition and a hemorrhagic area was also encapsulated in the cutting sections (Figure 3). Following the microscopic examination, the specimen was referred to the pathology laboratory and stained using hematoxylin and eosin (H&E) staining. As shown in Figure 4, a mixed erythrocytes, and hematopoietic cells with adipose tissue was detected, which is defined as the typical characteristic of myelolipoma (Figure 4).
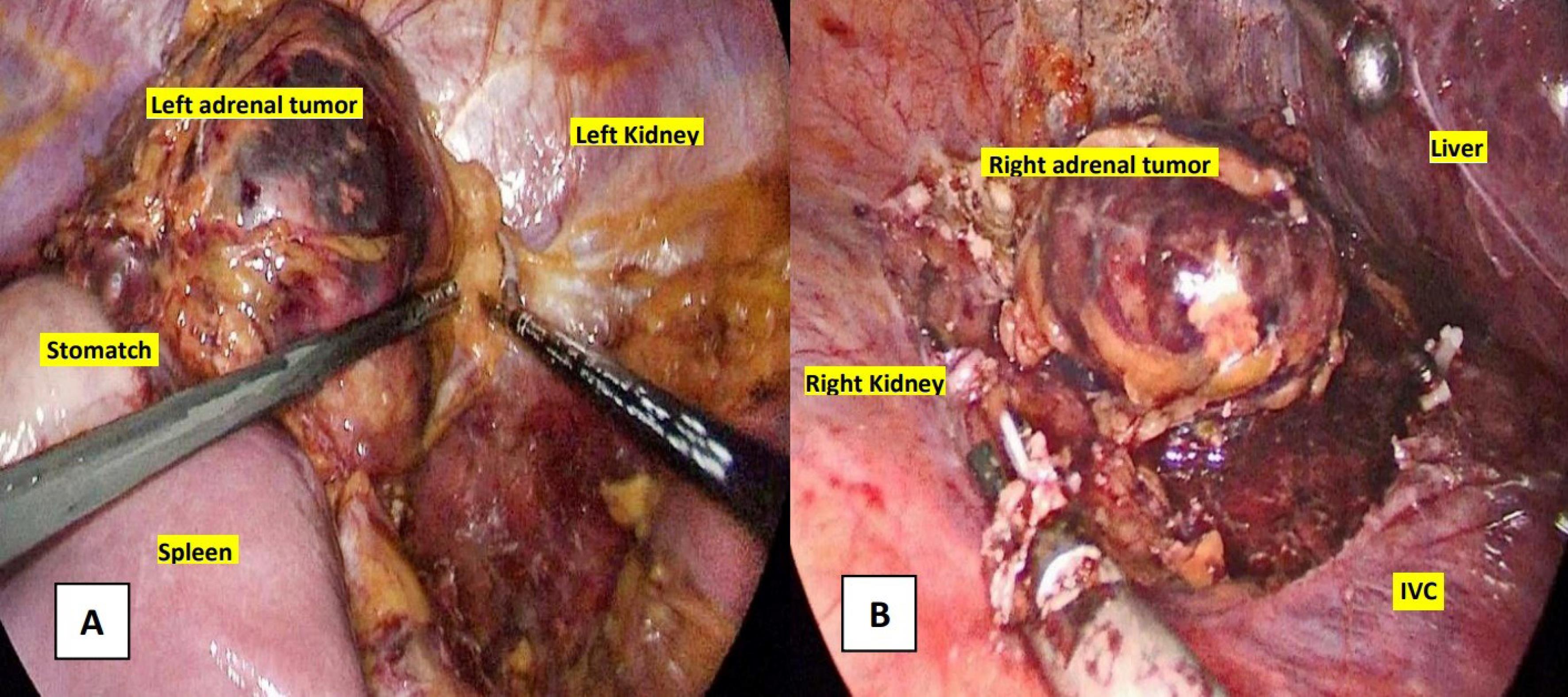
Figure 2.
Laparoscopic procedure. (A) Left adrenalectomy. (B) Right adrenalectomy
.
Laparoscopic procedure. (A) Left adrenalectomy. (B) Right adrenalectomy
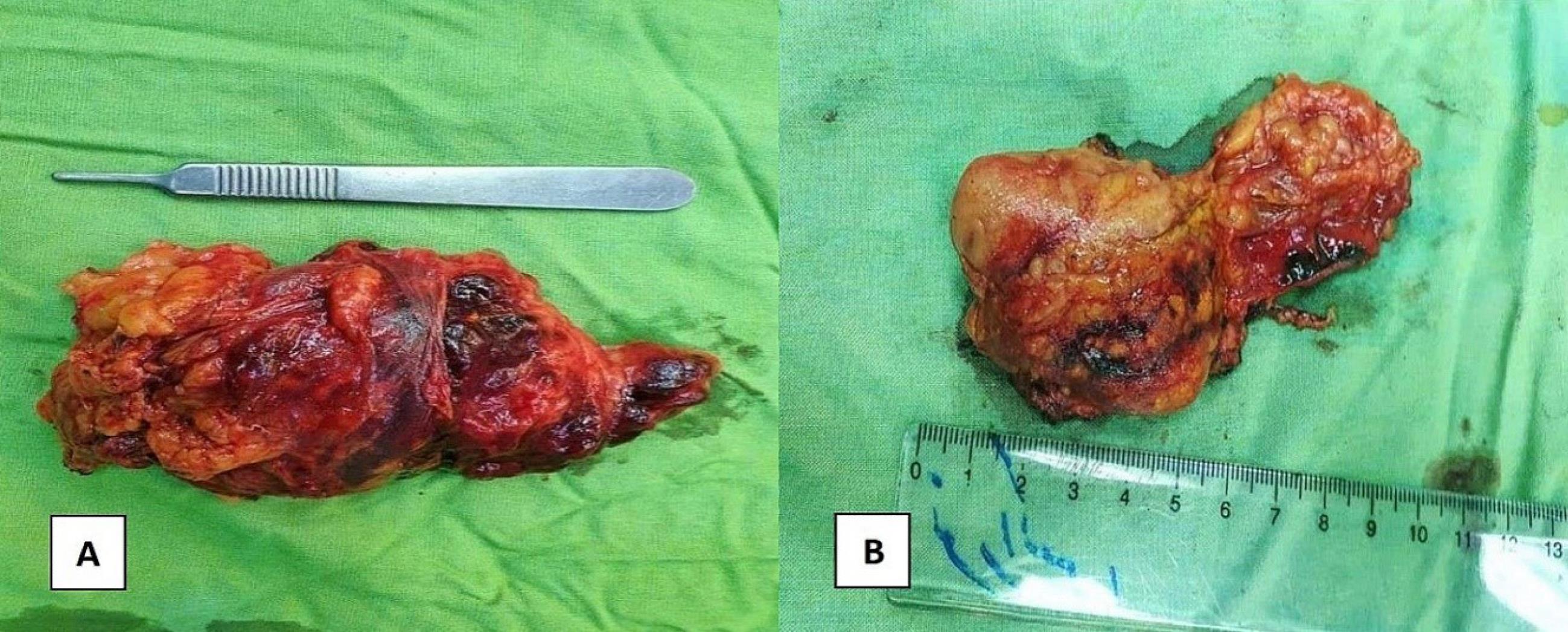
Figure 3.
A yellow-colored mass with a hemorrhagic area with the size of 60 × 50 × 40 mm in the left adrenal (A) and 35 × 30 × 10 mm in the right adrenal (B)
.
A yellow-colored mass with a hemorrhagic area with the size of 60 × 50 × 40 mm in the left adrenal (A) and 35 × 30 × 10 mm in the right adrenal (B)
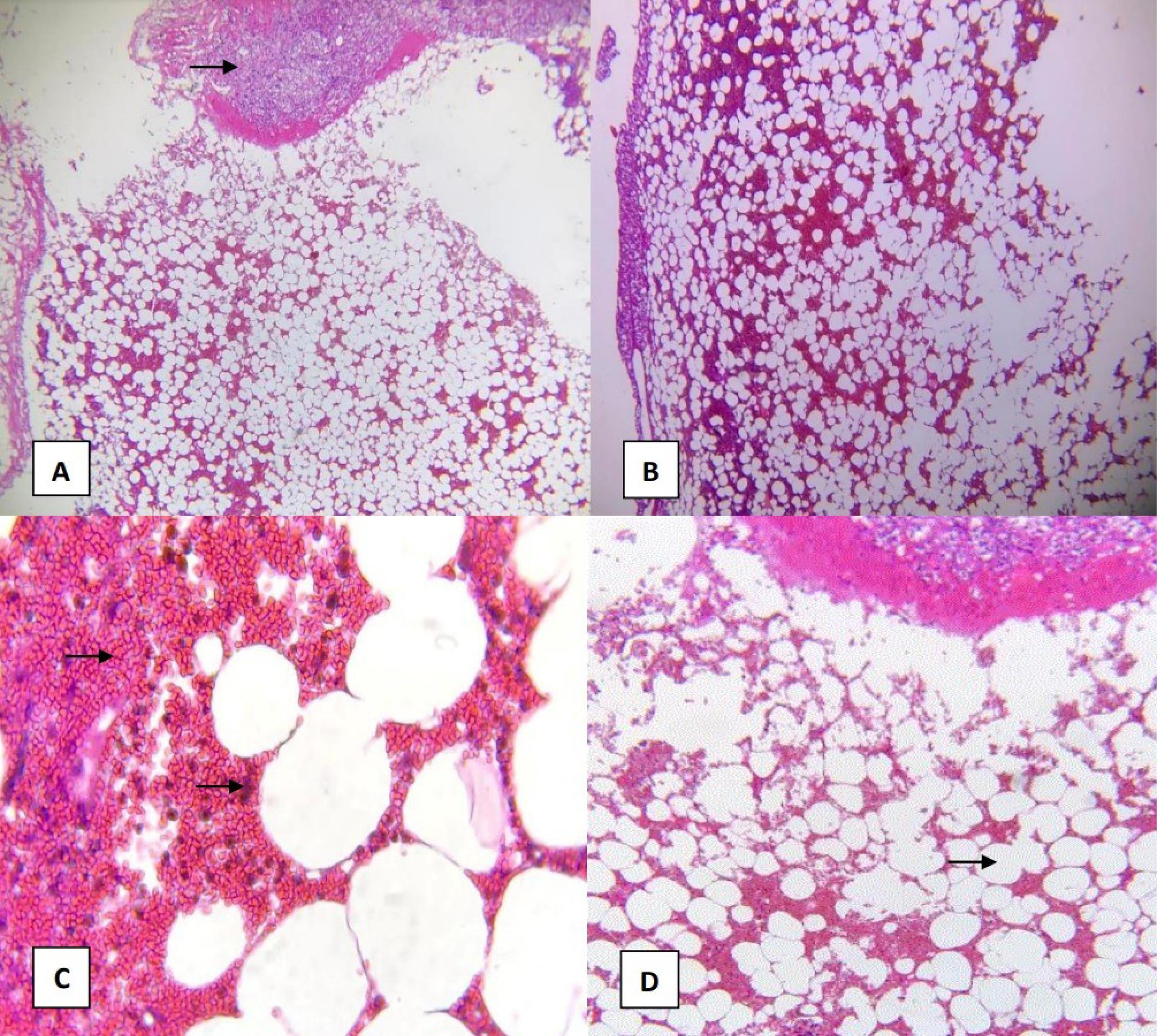
Figure 4.
Microscopic view of adrenal tissue stained by hematoxylin and eosin (H&E stain). The typical histological features of myelolipoma have been shown. The section illustrates adrenal tissue (A), red blood cells, and hematopoietic elements (C) admixed with adipose tissue (D)
.
Microscopic view of adrenal tissue stained by hematoxylin and eosin (H&E stain). The typical histological features of myelolipoma have been shown. The section illustrates adrenal tissue (A), red blood cells, and hematopoietic elements (C) admixed with adipose tissue (D)
The patient was in stable condition and was discharged on the second postoperative day. After six months of follow-up, the patient had no abdominal pain, hematuria, and inflammation-related complaints.
Discussion
Adrenal myelolipomas consist of adipose tissue with a combination of myeloid and erythroid tissues that were first described in 1905.9 Adrenal myelolipomas are usually non-functional, unilateral, and asymptomatic. Some studies have reported that bilateral adrenal myelolipomas occur in 10%-12% of patients.6 Adrenal myelolipomas may be implicated in endocrine dysfunction.10 However, there was no case report of hormone-secreting bilateral myelolipomas, so far.8 Bilateral myelolipomas may be symptomatic due to the effect of mass compression on adjacent tissues.11 Patients may also experience abdominal pain, renovascular hypertension, abdominal mass, and hematuria; moreover, they may become complicated with intraperitoneal hemorrhage and require emergent surgery.
Adrenal myelolipoma is usually observed in small sizes, and does not usually exceed 4–5 cm. The lesions larger than 8 cm are called giant tumors. The largest lesion ever reported in the adrenal gland was 31 × 24.5 × 11.5 cm.12 These tumors have been incidentally identified due to the extensive use of imaging modalities.1 Given the high-fat content of myelolipoma, it has a typic histological appearance in imaging examination, limiting the differential diagnosis. In other words, the histological changes that occurred in myelolipoma may affect CT scan findings.
Adrenal myelolipomas mainly exhibit small areas of adipose tissue in a soft tissue mass, whereas some types are composed exclusively of fat. Some areas with attenuation values less than −30 HU can be detected in practically all myelolipomas. In addition, myelolipomas may have low attenuation values due to a large amount of intracellular lipid, rarely less than −20 HU. The characteristic appearance of myelolipomas in the ultrasound is homogenous hyperechoic echogenicity with a regular margin.13 Moreover, it can be detected as a low attenuation lesion on CT scan and a hyperintense lesion in T1-weighted magnetic resonance imaging (MRI).14 Ultrasonography has also a limited role in assessing adrenal masses due to its low accuracy in detecting and classifying small adrenal neoplasms, compared to CT scan and MRI, resulting in the differentiation of a cystic mass from a solid mass. Contrast-enhanced CT is classified as the first-level imaging modality for evaluating adrenal lesions. It permits a quick execution that yields high spatial resolution, with findings of pre-contrast images and post-contrast behavior being frequently employed to achieve an accurate diagnosis.15
There is no substantial evidence of bilateral adrenal myelolipomas. Indeed, this report indicated a rare case of large bilateral myelolipomas, consisting of the 23 × 11 × 19 cm mass on the left side and 15 × 13 × 6.8 cm on the right side, respectively.16 In bilateral adrenal myelolipomas, observed in this case, the left lesion is larger than the right, which may be due to space constraints to viscera on the right side.17
Surgery is defined as the standard approach for the treatment of symptomatic or/and large adrenal lesions with neuroendocrine dysfunction.8 Noteworthy, laparoscopic surgery has also more benefits and is safe than open procedures.18 Lesions larger than 7–10 cm should be resected due to the feasibility of cancerous tissues, the probability of spontaneous rupture, and retroperitoneal hemorrhage.19 Some studies have also reported asymptomatic lesions less than 4 cm with bleeding and rupture. Moreover, patients should be followed for 6 to 12 months.20,21 Notable, these small tumors can grow during observation and bleeding after minor trauma.22 At first, it is suggested that the largest functional lesion(s) should be resected in patients with bilateral myelolipoma. The smaller contralateral mass could be also conservatively managed to spare the patient from lifelong glucocorticoid replacement therapy.4
Conclusion
Adrenal myelolipomas are rare and benign endocrine tumors that are often incidentally identified using imaging modalities. The laparoscopic excision is the standard approach for treating either symptomatic or large asymptomatic lesions. Histopathology examination is the only way to confirm the diagnosis of adrenal myelolipomas. Reporting such cases has a crucial impact on promoting clinical suspicion and achieving a consensus regarding the management of rare tumors.
Acknowledgments
Thanks to all the participants in this article.
Competing Interests
The authors declared that they have no conflicts of interest.
Data Availability Statement
All generated or analyzed data are included in this article and are available at the Department of Cardiothoracic Surgery, Imam Reza Hospital, Tabriz University of Medical Sciences, Tabriz, Iran.
Ethical Approval
This study was approved by the Ethics Committee of Tabriz University of Medical Sciences under protocol number IR.TBZMED.REC.1400.747.
References
- Scalisi G. Editorial comment to adrenal myelolipoma associated with hyperandrogenemia. Int J Urol 2012; 19(11):1029-30. doi: 10.1111/j.1442-2042.2012.03122.x [Crossref] [ Google Scholar]
- Farashi E, Rasihashemi SZ, Halimi M. Large Adrenal Ganglioneuroma Presenting with Clinical Pheochromocytoma: A Rare Case Report. Case Rep Clin Pract 2022; 7(4):167-71. doi: 10.18502/crcp.v7i4.11590 [Crossref] [ Google Scholar]
- Wale DJ, Wong KK, Viglianti BL, Rubello D, Gross MD. Contemporary imaging of incidentally discovered adrenal masses. Biomed Pharmacother 2017; 87:256-62. doi: 10.1016/j.biopha.2016.12.090 [Crossref] [ Google Scholar]
- Daneshmand S, Quek ML. Adrenal myelolipoma: diagnosis and management. Urol J 2006; 3(2):71-4. [ Google Scholar]
- Naidu V, Singh B. Adrenal lesions encountered in current medical practice− a review of their radiological imaging. SA J Radiol 2013; 17(4):128-38. doi: 10.7196/sajr.914 [Crossref] [ Google Scholar]
- Doddi S, Singhal T, Leake T, Sinha P. Management of an incidentally found large adrenal myelolipoma: a case report. Cases J 2009; 2:8414. doi: 10.4076/1757-1626-2-8414 [Crossref] [ Google Scholar]
- Kenney PJ, Wagner BJ, Rao P, Heffess CS. Myelolipoma: CT and pathologic features. Radiology 1998; 208(1):87-95. doi: 10.1148/radiology.208.1.9646797 [Crossref] [ Google Scholar]
- Zattoni D, Balzarotti R, Rosso R. The management of bilateral myelolipoma: case report and review of the literature. Int J Surg Case Rep 2015; 12:31-6. doi: 10.1016/j.ijscr.2015.04.021 [Crossref] [ Google Scholar]
- Gierke E. Über Knochenmarksgewebe in der Nebenniere. Beitr Path Anat Supple 1905; 7:311. [ Google Scholar]
- Hisamatsu H, Sakai H, Tsuda S, Shigematsu K, Kanetake H. Combined adrenal adenoma and myelolipoma in a patient with Cushing’s syndrome: case report and review of the literature. Int J Urol 2004; 11(6):416-8. doi: 10.1111/j.1442-2042.2004.00815.x [Crossref] [ Google Scholar]
- de Jesús Garduño-García J, Arjona Villicana R, Pimentel L, Pérez Díaz I, Gómez-Pérez FJ. Late-occurring giant adrenal myelolipoma in a patient with congenital adrenal hyperplasia. Endocrinol Nutr 2013; 60(9):e33-4. doi: 10.1016/j.endonu.2012.09.017 [Crossref] [ Google Scholar]
- Akamatsu H, Koseki M, Nakaba H, Sunada S, Ito A, Teramoto S. Giant adrenal myelolipoma: report of a case. Surg Today 2004; 34(3):283-5. doi: 10.1007/s00595-003-2682-4 [Crossref] [ Google Scholar]
- Fan J, Tang J, Fang J, Li Q, He E, Li J. Ultrasound imaging in the diagnosis of benign and suspicious adrenal lesions. Med Sci Monit 2014; 20:2132-41. doi: 10.12659/msm.890800 [Crossref] [ Google Scholar]
- Gupta P, Bhalla A, Sharma R. Bilateral adrenal lesions. J Med Imaging Radiat Oncol 2012; 56(6):636-45. doi: 10.1111/j.1754-9485.2012.02435.x [Crossref] [ Google Scholar]
- Albano D, Agnello F, Midiri F, Pecoraro G, Bruno A, Alongi P. Imaging features of adrenal masses. Insights Imaging 2019; 10(1):1. doi: 10.1186/s13244-019-0688-8 [Crossref] [ Google Scholar]
- McGeoch SC, Olson S, Krukowski ZH, Bevan JS. Giant bilateral myelolipomas in a man with congenital adrenal hyperplasia. J Clin Endocrinol Metab 2012; 97(2):343-4. doi: 10.1210/jc.2011-2373 [Crossref] [ Google Scholar]
- Al-Bahri S, Tariq A, Lowentritt B, Nasrallah DV. Giant bilateral adrenal myelolipoma with congenital adrenal hyperplasia. Case Rep Surg 2014; 2014:728198. doi: 10.1155/2014/728198 [Crossref] [ Google Scholar]
- Castillo OA, López-Fontana G, Vitagliano G. Laparoscoscopic synchronous bilateral adrenalectomy. Arch Esp Urol 2011; 64(2):114-20. [ Google Scholar]
- Ioannidis O, Papaemmanouil S, Chatzopoulos S, Paraskevas G, Konstantara A, Kotronis A. Giant bilateral symptomatic adrenal myelolipomas associated with congenital adrenal hyperplasia. Pathol Oncol Res 2011; 17(3):775-8. doi: 10.1007/s12253-010-9330-2 [Crossref] [ Google Scholar]
- Amendolara M, Barbarino C, Bucca D, Guarnieri F, Novello GB, Romano FM, et al. [Giant and bilateral adrenal myelolipoma. Case report]. G Chir 2008;29(3):85-8. [Italian].
- Cha JS, Shin YS, Kim MK, Kim HJ. Myelolipomas of both adrenal glands. Korean J Urol 2011; 52(8):582-5. doi: 10.4111/kju.2011.52.8.582 [Crossref] [ Google Scholar]
- Russell C, Goodacre BW, vanSonnenberg E, Orihuela E. Spontaneous rupture of adrenal myelolipoma: spiral CT appearance. Abdom Imaging 2000; 25(4):431-4. doi: 10.1007/s002610000061 [Crossref] [ Google Scholar]