J Res Clin Med. 12:14.
doi: 10.34172/jrcm.32240
Systematic Review
Effectiveness of transcutaneous electrical nerve stimulation (TENS) modality for treating myofascial pain syndrome: A systematic review and meta-analysis
Vahideh Toopchizadeh Conceptualization, Funding acquisition, Supervision, Validation, Visualization, Writing – review & editing, 1 
Behzad Izadseresht Investigation, Writing – original draft, Writing – review & editing, 1
Bina Eftekharsadat Data curation, Funding acquisition, Supervision, Validation, Visualization, Writing – review & editing, 1 
Hanieh Salehi-Pourmehr Formal analysis, Investigation, Methodology, Resources, Software, 2, * 
Sanam Dolati Investigation, Project administration, Supervision, Writing – original draft, Writing – review & editing, 1, * 
Author information:
1Physical Medicine and Rehabilitation Research Center, Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
2Research Center for Evidence-Based Medicine, Iranian EBM Centre: A Joanna Briggs Institute (JBI) Center of Excellence, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Introduction:
Myofascial pain syndrome (MPS) is a prevalent chronic pain disorder that initiates from myofascial trigger points (MTrPs) in skeletal muscle. This study aimed to systematically review the studies on the efficiency of transcutaneous electrical nerve stimulation (TENS) on MPS.
Methods:
The data from PubMed, EMBASE, Web of Science, and Cochrane Central Register of Controlled Trials from the database inception to July 2021 were used. Two reviewers screened the papers independently, and took out the data based on the PRISMA protocol. Information associated with the study was gathered, including glocation, time, author, modality, details of comparisons between groups, duration of treatment, participants’ characteristics, and duration of follow-up.
Results:
Among 422 articles, a total of 21 articles met the exclusion and inclusion criteria for the study (including 12 trials) and 7 for meta-analysis. The overall estimated effect showed a significant decrease in Visual analog scale (VAS) score in the TENS group compared with the exercise group (MD=-1.60, 95% CI: -2.16 to -1.05, P<0.00001). However, there was no significant decrease in pain pressure threshold (PPT) score in the TENS group compared with sham (MD=1.88, 95% CI: -0.62 to 4.38, P=0.14) or exercise (MD=0.19, 95% CI: -0.99 to 1.37, P=0.75). TENS therapy did not improve the PPT score (MD=0.96, 95% CI: -0.72 to 2.64, P=0.26).
Conclusion:
The published evidence for the treatment of MPS by TENS has been reviewed. TENS can be utilized as an adjuvant treatment to help alleviate MPS but should not be regarded as a monotherapy.
Keywords: Myofascial pain syndrome, Pain management, TENS
Copyright and License Information
© 2024 The Authors.
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
Not applicable.
Introduction
Myofascial pain syndrome (MPS) is a type of chronic pain syndrome that appears in muscles, fascia, or related soft tissues and can be along with apparent emotional disorders or dysfunctions.1 MPS is a regional pain disorder and a relapsing disease that affects every age group and is characterized by the presence of trigger points (TrPs) within muscles or fascia.2 The predilection sites of MPS are the neck, shoulders, and back. About 30.0%-93.0% of the patients with musculoskeletal pain are exposed to MPS.3 Since there are many different treatment options accessible for MPS, treatment strategies should meet the lesion site, course of disease, and individual situation.4 At present, pharmacologic interventions consist of muscle relaxants such as benzodiazepines, tizanidine, and cyclobenzaprine; Tricyclic antidepressants (TCAs), and topical agents such as diclofenac gel and lidocaine patches, in addition to injection therapy of Botox or lidocaine are frequently used for pain relief in MPS. Other modalities including acupuncture, dry needling, and to a certain extent transcutaneous electrical nerve stimulation (TENS) therapy have been employed to help alleviate the chronic pain in MPS.5 TENS is the transcutaneous and noninvasive use of electrical stimulation to produce analgesia.6 It effectively improves pain in patients with MPS, and is theorized for increasing the release of endogenous opiates (enkephalins and β-endorphins), stimulating sensory nerves and gate-control mechanisms, modulating autonomic responses, and partly blocking C-fibers for pain relief.7 Conventional TENS applications were effective in pain relief and range of motion in patients with MPS.8
Systematically, we reviewed the information from randomized controlled trials (RCTs) and quasi-RCTs to assess of the efficiency of TENS modality in treating myofascial pain. Understanding the actual benefit of this modality is important clinically since it may help to develop good rehabilitation protocols for chronic MPS circumstances.
Methods
Study design
This systematic review was performed based on the predetermined guidelines presented by the Cochrane Collaboration (2008).9
Studies
All RCTs and quasi RCTs were included.
Participants
Inclusion criteria
All relevant studies involved patients with MPS, and sought treatment with the following modality: TENS.
Exclusion criteria
-
Articles with no adequate patients (fewer than seven patients)
-
All retrospective studies
-
Studies with no access to full-text
-
Withdrawn trials.
Interventions
TENS (transcutaneous electrical nerve stimulation).
Types of comparisons
The quantitative component of this review was considered placebo, sham controls, and other conventional controls including exercise.
Types of outcomes
Primarily, our objective was to assess the efficiency of TENS in pain relief. Visual analog scale (VAS) was included in valid reliable common scales for pain intensity evaluation and monitoring. The primary outcome was the efficacy of each modality using pain reduction according to the VAS questionnaire and pain pressure threshold (PPT) (using a Pressure Algometer).
Table 1 presents PICOS criteria for exclusion and inclusion of studies.
Table 1.
PICOS criteria for inclusion and exclusion of studies
|
Parameter
|
|
| Participants |
Patients with Myofascial pain syndrome |
| Intervention |
Transcutaneous electrical nerve stimulation |
| Comparator |
Placebo, sham or conventional methods including exercise. |
| Outcomes |
Any beneficial effect on Pain reduction (using VAS questionnaire), and pain pressure threshold (using Pressure Algometer) |
| Study design |
Randomized controlled trials (RCTs) or quasi-experimental studies. |
The strategy of article search
A systematic search was conducted in Cochrane Library, ProQuest, Clinicaltrial.gov, Web of Science, Google Scholar, Ovid, PubMed, and Scopus databases in July 2021. The studies were searched based on the keywords in line with the MeSH glossary. The review search ahead of published or printed articles was performed irrespective of time limitations or language. References accessible in review articles were assessed as further resources. Persian thesis was reviewed by searching the universities’ websites. It also tried to search for articles available at conferences. However, no full access was found to the gray literature.
Data collection and analysis
Selecting the studies
The abstracts and titles of all studies recognized by the search approach were read independently by two authors. Once all potentially related articles were retrieved, the full text of each article was independently evaluated by each reviewer for inclusion and then methodological quality and acceptability of selected studies were assessed through the Cochrane appraisal risk of bias checklist. When there was not any consistency, the idea of the third author was considered and agreed upon.
Assessing the risk of bias
The articles were reviewed regarding selection detection, performance bias, reporting, and attrition bias. Also, an assessment was separately performed by two authors in terms of the Cochrane Handbook. The considered items included Random sequence generation (assessing for probable selection bias); allocation concealment (checking for potential selection bias); blinding of participants and personnel (assessing for possible performance bias); blinding of outcome assessment (checking for possible detection bias); selective reporting (checking for reporting bias), incomplete outcome data (assessing for possible attrition bias); and other bias.10 In all cases, a “low risk” assessment represented a low rate of bias, assessing “high risk” means a high rate of bias, and evaluating “unclear risk” represents the uncertain risk of bias.
Data extraction and management
Data were extracted using a form. Information associated with the study was gathered, including time, author, place, modality, comparison details between groups, treatment duration, follow-up duration, and participants’ characteristics. The reports were summarized for studies published more than once, and those published with the most complete information were included in the study. These data were used for the results published only in older versions. All differences between the published versions must be considered. The information needed by the original author was requested via correspondence and the associated data was achieved. Disagreement was resolved through consultation with the third party, who is an expert in this field.
Data analysis
Owing to failure in quasi-experimental articles or complete report data, or a control arm rather than the placebo, sham, or conventional methods, meta-analysis was possible only on 16 articles.
Meta-analysis was performed through Review Manager 5.4.1 statistical software. The findings of the per-protocol analysis were utilized for meta-analysis for intention-to-treat analysis but the results were not reported. Here, all the results were quantitative. Moreover, mean and standard deviation were utilized for analysis before and after the intervention. Using standard deviation and mean changes in each group followed by the intervention in comparison with the baseline, and then, MD changes were calculated with a confidence interval of 95%. In this regard, mean changes from baseline was calculated by this formula:
Mean change = mean of follow-up measurement – mean of baseline measurement
To obtain standard deviation (SD) changes, the previously reported formula was used.11
The quantity of heterogeneity amongst the included studies’ results was assessed by the I2 index indicating the variability percentage between studies. A value of more than 50% for this index, represents the higher heterogeneity. Finally, the meta-analysis was reported using a random effect. In addition, for heterogeneity less than 50%, the fixed-effect model was used for analysis. Through the forest plot, pooled results were presented, in case of at least two articles.
Results
Results of the search
In the first phase, 422 articles were collected from databases, and after eliminating the duplicated items, 365 articles remained. Then, the articles were assessed according to the inclusion criteria. Considering non-relevance to this review, 340 were excluded based on the abstract and title. Ultimately, out of 25 articles, 21 were included in systematic review (including 12 trials),8,12-31 and seven of them for meta-analysis.8,12,13,15-18 (Figure 1).
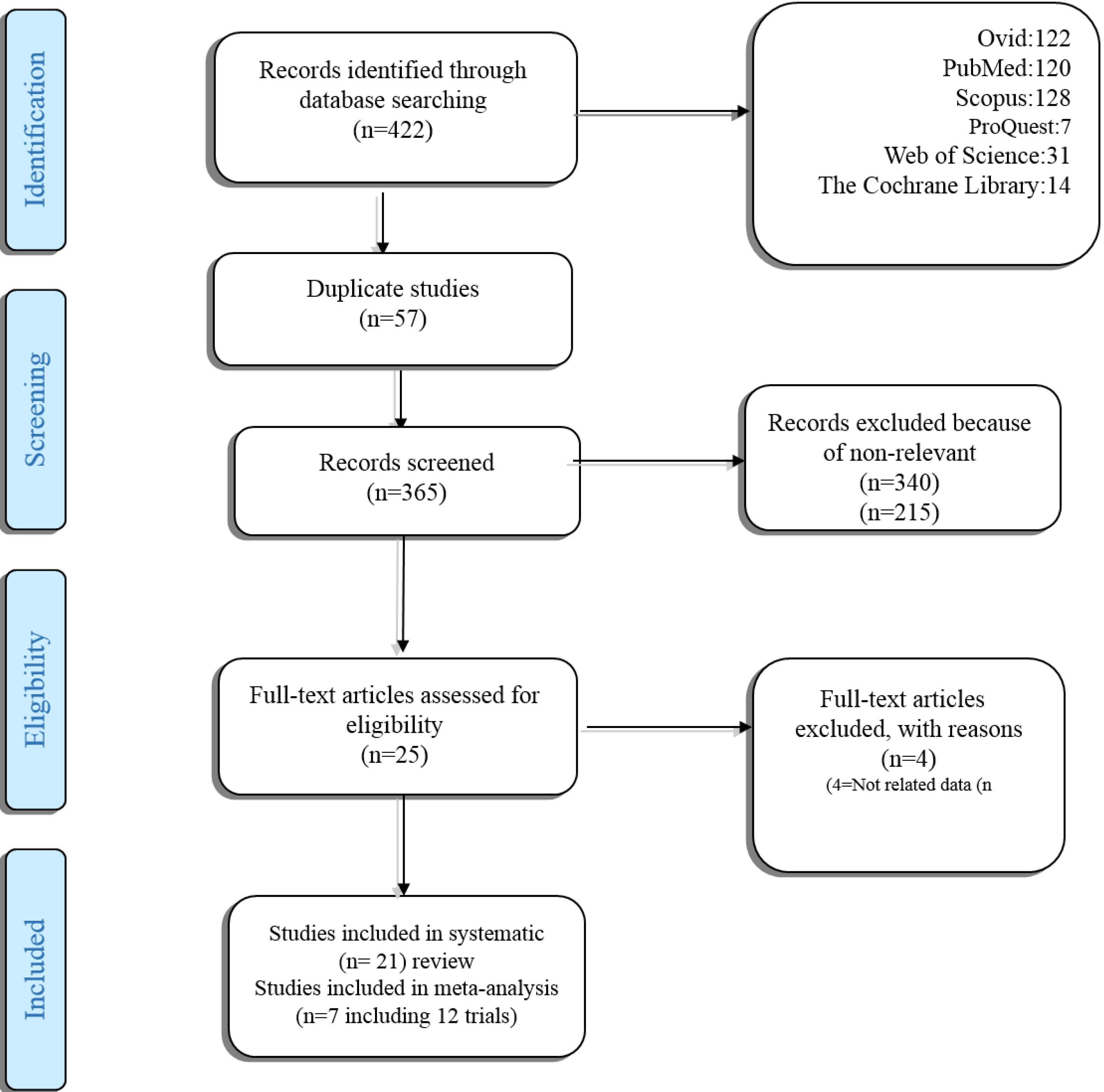
Figure 1.
Search and selection process of systematic review
.
Search and selection process of systematic review
Explanation of studies
All of the studies included in this systematic work published from 2002 to 2021, were clinical trials, and included a control group with a parallel arm or cross-over design. Of these, 17 were conducted in Turkey; the others were in India, Iran, South Korea, Taiwan, Thailand, USA, UK, Egypt, etc (Table 2).
Table 2.
Characteristics of the included studies
|
Author
|
Year
|
Type of study
|
Country
|
Modality
|
Control group modality
|
Case
|
Control
|
Mean age
|
Male
|
Female
|
| Hou15 |
2002 |
RCT |
Taiwan |
Group 1: ischemic compression ± TENS Group 2: exercise ± TENS |
Exercise |
Group 1: 9
Group 2: 9 |
21 |
46.89 ± 14.91 and 51.00 ± 16.19 |
8 |
31 |
| Ardiç8 |
2002 |
RCT |
Turkey |
Group 1: TENS
Group 2: EMS |
Exercise |
Group 1:15
Group 2:15 |
10 |
41.73 ± 8.04 and 42.60 ± 9.40 |
4 |
36 |
| Smania28 |
2005 |
RCT |
Italy |
TENS |
Placebo |
18 |
18 |
36.56 ± 14.94 and 44.61 ± 16.62 |
11 |
25 |
| Gemmell14 |
2010 |
Double-blind, randomized placebo-controlled trial |
UK |
TENS |
Sham TENS |
30 |
30 |
24.2-25.6 |
27 |
28 |
| Sahin17 |
2011 |
Randomized, placebo-controlled clinical trial |
Turkey |
Group 1: conventional TENS Group 2: conventional TENS Group 3: Burst TENS |
Sham TENS |
Group 1: 19
Group 2: 18
Group 3: 19 |
19 |
18-65 |
35 |
40 |
| Rodríguez-Fernández16 |
2011 |
Single blind randomized trial |
Spain |
TENS |
Sham TENS |
38 |
38 |
18-41 |
45 |
31 |
| Ramanathan19 |
2015 |
RCT |
India |
US and TENS |
Exercise |
15 |
15 |
|
|
|
| Azatcam12 |
2016 |
Randomized, controlled, single- blind, prospective study |
Turkey |
TENS |
Exercise |
23 |
23 |
18-65 |
21 |
48 |
| Kim32 |
2016 |
Single-blind RCT |
Korea |
US |
Exercise (therapeutic inflatable ball) |
18 |
22 |
67.71 ± 5.65 and 71.15 ± 5.06 |
5 |
40 |
| Dissanayake 33 |
2016 |
Single-blind RCT |
Sir Lanka |
Group 1: TENS
Group 2: IFT |
Hot pack, active range of motion exercises, myofascial release, and a home exercise program with postural advice |
Group 1: 35
Group 2: 35 |
35 |
18-55 |
47 |
58 |
| Takla18 |
2018 |
RCT |
Egypt |
G1: burst-TENS-CT: burst transcutaneous electrical nerve stimulation combined therapy, G2: AMF-CT |
Sham TENS |
Group 1:23
Group 2:25 |
22 |
34.39 ± 5.92 and 34.88 ± 5.67 and 35.18 ± 5.56 |
30 |
40 |
| Jeon34 |
2012 |
RCT |
Korea |
ESWT |
TPI + TENS |
15 |
15 |
G1:40.86 ± 13.07; G2:45.00 ± 15.46 |
G1:13; G2:9 |
G1:2; G2:6 |
| Kim24 |
2014 |
RCT |
Korea |
G1: NSAID patch, G2: NSAID patch + TENS, G3: NSAID patch + heating pad, and G4: NSAID patch + topical capsaicin |
G1:25; G2:24; G3:25; G4:25 |
- |
- |
G1:44.76 ± 12.71; G2:49.17 ± 13.52; G3:47.56 ± 10.67; G4:48.88 ± 11.11 |
- |
- |
| León-Hernández25 |
2014 |
RCT |
Spain |
Needling + TENS |
Needling |
31 |
31 |
26.81 ± 9.63; G2: 23.32 ± 4.77 |
G1:7; G2:9 |
G1:24; G2:22 |
| Chalkoo21 |
2015 |
RCT |
India |
G1: conventional treatment including muscle relaxants, analgesics, soft diet, and hot fomentations; G2: TENS; G3: combined conventional and TENS treatment |
Placebo |
each 15 |
15 |
17-60 |
23 |
37 |
| Amjad 20 |
2016 |
RCT |
Pakistan |
TENS |
US |
32 |
32 |
G1:32 ± 1; G2:37 ± 9.9 |
25 |
39 |
| Rai 27 |
2016 |
RCT |
India |
G1: TENS; G2:US |
control |
30;30 |
30 |
G1:29.73 ± 8.804; G2:32 ± 10.174; G3:34.93 ± 12.57 |
6;7;12 |
24;23;18 |
| Khalifeh 23 |
2018 |
RCT |
Iran |
G1: TENS + pharmacotherapy; G2: LLLT; G3: sham LLLT |
G1:18; G2:19 |
18 |
18-60 |
|
|
| Mansourian 26 |
2018 |
RCT |
Iran |
TENS + medication |
LLLT + medication; medication |
36 |
36, 36 |
21-60 |
18.54% |
81.46% |
| Chiou 22 |
2019 |
RCT |
Taiwan |
TENS on the acupuncture point |
TENS on trigger point |
30 |
30 |
G1: 42.13 (12.93); G2: 41.98 (15.04) |
G1: 25; G2: 23 |
G1: 5; G2:7 |
| Gezgİnaslan 31 |
2020 |
Prospective, randomized, single-blind clinical study |
Turkey |
ESWT |
US, HP, TENS group |
49 |
45 |
44.2 ± 11.94 |
16 |
78 |
AMF-CT, amplitude modulated frequency combined therapy; LLLT, low-level laser therapy; IFT, interferential therapy; TENS, transcutaneous electrical nerve stimulation; ESWT, extracorporeal shock wave therapy; US, Ultrasound; HP, hot pack; BNR, Beam Nonuniformity Ratio; ERA, effective radiating area; GP, Group
Meta-analysis was performed only on seven articles8,12,13,15-18 (including 12 trials) owing to failure to completely report data or quasi-experimental articles, or a control arm rather than the placebo, sham, or conventional methods,
The outcome measurement tools were VAS, PPT, or both, and a minority of studies used a numeric pain rating scale, Nottingham Health Profile, or neck pain disability index to report their outcomes. Total sessions were varied between 1-30 as well as one to seven sessions per week. The included studies’ modification was continuous, biphasic, or Burst/conventional. The frequency (MHz), effective radiating area (ERA) (cm2), Beam Nonuniformity Ratio (BNR), output (W/cm2), and duty cycle (%) are summarized in Tables 3 and 4.
Table 3.
Characteristics of the used modality
|
Author
|
Year
|
Modification
|
Frequency (MHz)
|
ERA (cm2)
|
BNR
|
Output (W/cm2)
|
Duty cycle%
|
Total session
|
Sessions per week
|
| Hou15 |
2002 |
Biphasic |
- |
- |
- |
- |
- |
14 |
7 |
| Ardiç8 |
2002 |
Biphasic |
- |
- |
- |
- |
- |
1 |
1 |
| Smania28 |
2005 |
Biphasic |
- |
- |
- |
- |
- |
10 |
5 |
| Gemmell14 |
2010 |
|
- |
- |
- |
- |
- |
1 |
1 |
| Sahin17 |
2011 |
Burst/
conventional |
- |
- |
- |
- |
- |
|
|
| Rodríguez-Fernández16 |
2011 |
Burst |
- |
- |
- |
- |
- |
1 |
1 |
| Ramanathan 19 |
2015 |
Pulse/burst |
1 |
|
|
1.5 |
|
30 |
5 |
| Azatcam12 |
2016 |
Biphasic |
|
|
|
|
|
10 |
5 |
| Kim32 |
2016 |
Continuous |
1 |
40 |
|
1 |
100 |
8 |
2 |
| Dissanayake33 |
2016 |
Biphasic |
|
|
|
|
|
8 |
2 |
| Takla18 |
2018 |
Group 1: Burst TENS
Group 2: AMF TENS |
- |
- |
- |
- |
- |
12 |
3 |
| Jeon34 |
2012 |
|
- |
- |
- |
- |
- |
|
|
| Kim 24 |
2014 |
|
- |
- |
- |
- |
- |
2 |
2 |
| León-Hernández25 |
2014 |
Conventional |
2 |
- |
- |
- |
- |
3 |
2 |
| Chalkoo21 |
2015 |
Conventional |
10 Htz |
- |
- |
- |
- |
3 |
3-day interval |
| Amjad20 |
2016 |
Conventional-continuous |
1 |
- |
- |
1.5 |
- |
12 |
|
| Rai27 |
2016 |
Conventional |
- |
- |
|
0.73 |
- |
12 |
3 times every 2 weeks |
| Khalifeh 23 |
2018 |
- |
- |
- |
|
200 mW/cm2 |
- |
10 |
two times a week |
| Mansourian26 |
2018 |
- |
- |
- |
|
- |
- |
10 |
3 |
| Chiou22 |
2019 |
- |
0.6/60 Hz |
- |
- |
- |
- |
7 |
Seven consecutive days |
| Gezgİnaslan31 |
2020 |
- |
- |
- |
- |
1.5 |
- |
7 |
Three days interval |
AMF, amplitude modulated frequency; TENS, transcutaneous electrical nerve stimulation; ESWT, extracorporeal shock wave therapy; US, Ultrasound; HP, hot pack; BNR, Beam Nonuniformity Ratio; ERA, effective radiating area
Table 4.
The outcomes measure tools and results
|
Author
|
Intervention group
|
Control group
|
|
VAS (pre)
|
VAS (post)
|
PPT (pre)
|
PPT (post)
|
VAS (pre)
|
VAS (post)
|
PPT (pre)
|
PPT (post)
|
| Hou15 |
Group 1: 4.69 ± 2.24 Group 2: 4.68 ± 1.28 |
Group 1: 2.46 ± 1.33 Group 2: 2.43 ± 0.65 |
Group 1: 2.68 ± 0.75 Group 2: 3.09 ± 1.10 |
Group 1: 3.39 ± 0.83 Group 2: 3.93 ± 1.03 |
5.10 ± 1.78 |
4.33 ± 1.82 |
3.07 ± 0.96 |
3.45 ± 1.09 |
| Ardiç8 |
Group 1: 7.40 ± 1.88 Group 2: 7.00 ± 1.20 |
Group 1: 4.27 ± 2.28 Group 2: 4.13 ± 2.59 |
Group 1: 2.00 ± 0.76 Group 2: 2.00 ± 0.85 |
Group 1: 0.80 ± 0.68 Group 2: 1.07 ± 0.59 |
7.50 ± 1.84 |
6.50 ± 2.55 |
2.10 ± 0.74 |
1.70 ± 0.95 |
| Smania28 |
Range: 40-50 |
Range:30-40 |
|
|
Range:40-50 |
Range:40-50 |
|
|
| Gemmell14 |
|
|
4.0 ± 1.4 |
3.51 |
|
|
4.0 ± 1.4 |
3.55 |
| Sahin17 |
Group 1:7.12 ± 1.87 Group 2:6.15 ± 1.18 Group 3:6.85 ± 1.35 |
Group 1: 6.85 ± 1.55 Group 2: 6.55 ± 1.42 Group 3: 6.10 ± 2.15 |
|
|
7.56 ± 1.17 |
6.95 ± 1.15 |
|
|
| Rodríguez-Fernández16 |
|
|
2.1 ± 0.5 |
2.7 ± 0.7 |
|
|
2.2 ± 0.8 |
2.2 ± 0.8 |
| Ramanathan19 |
7.06 ± 0.798 |
5.93 ± 0.703 |
|
|
7.13 ± 0.833 |
3.60 ± 0.828 |
|
|
| Azatcam12 |
7.39 ± 0.66 |
1.78 ± 0.74 |
16.75 ± 2.34 |
24.12 ± 3.02 |
7.21 ± 0.51 |
2.95 ± 0.97 |
16.75 ± 1.94 |
22.82 ± 3.39 |
| Kim32 |
5.31 ± 1.52 |
2.67 ± 1.82 |
2.07 ± 0.70 |
2.45 ± 0.87 |
6.15 ± 1.62 |
3.34 ± 1.95 |
1.92 ± 0.34 |
2.50 ± 0.04 |
| Dissanayake33 |
Group 1:69.9 ± 2.8 Group 2:67.2 ± 8.7 |
Group 1: 45.3 ± 8.4 Group 2: 31.8 ± 6.2 |
|
|
70.3 ± 4.2 |
17.6 ± 3.1 |
|
|
| Takla18 |
|
|
Group 1: 0.27 ± 0.18 Group 2: 0.75 ± 0.16 |
Group 1: 4.57 ± 0.57 Group 2: 2.73 ± 0.35 |
|
|
0.71 ± 0.16 |
1.86 ± 0.17 |
| Jeon34 |
6.86 ± 0.90 |
1.86 ± 0.69 |
6.86 ± 1.35 |
12.57 ± 0.72 |
7.20 ± 1.30 |
2.80 ± 0.84 |
6.20 ± 1.92 |
9.60 ± 2.19 |
| Kim24 |
|
|
G1: 2.47 ± 0.83; G2: 2.79 ± 1.41; G3: 2.67 ± 0.74; G4: 2.59 ± 0.89 |
|
G1:2.42 ± 1.00; G2:2.94 ± 1.12; G3:3.01 ± 0.82; G4:2.89 ± 0.83 |
|
|
|
| León-Hernández25 |
4.82 ± 1.83 |
2.00 (1.00 and 5.00) |
1.80 ± 0.90 |
1.70 (1.18 and 6.75) |
4.82 ± 1.91 |
2.50 (1.00 and 4.00) |
1.72 ± 0.81 |
1.50 (1.15 and 1.87) |
| Chalkoo 21 |
G1: 3.7 (1.05); G2:4.0 (1.07); G3: 5.0 (1.31) |
G1: 0.6 (0.91); G2: 1.4 (0.91); G3: 0.1 (0.35) |
|
|
4.1 (0.64) |
4.1 (0.83) |
|
|
| Amjad 20 |
6 times a week for two weeks. |
|
|
|
|
|
|
|
| Rai27 |
240.60 ± 25.75 |
32.37 ± 13.02 |
|
|
247.87 ± 26.53 |
20.87 ± 6.35 |
|
|
| Khalifeh23 |
Trapezius: G1: 1.926 ± 1.777; G2: 2 ± 1.763 |
G1: 1.515 ± 0.812; G2: 1.444 ± 1.423 |
|
|
1.833 ± 2.526 |
2.666 ± 2.894 |
|
|
| Mansourian26 |
4.13 ± 1.75 |
4.77 ± 0.27 |
|
|
G1: 4.09 ± 1.76; G2: 2.87 ± 0.98 |
G1: 4.90 ± 0.27; G2: 5.01 ± 0.27 |
|
| Chiou22 |
6.70 (1.18) |
2.93 (1.64) |
|
|
6.20 (1.35) |
3.10 (1.42) |
|
|
| Gezgİnaslan31 |
8.3 ± 1.2 |
3.7 ± 1.7 |
|
|
8.1 ± 1.3 |
6.5 ± 1.2 |
|
|
Risk of bias in articles
Considering the Cochrane appraisal risk of bias checklist, all of the published articles included in the meta-analysis had moderate or good quality (Figures 2 and 3).
Effectiveness of TENS on pain relief
Fifteen RCTs used the TENS modality in one of the experimental or control arms, or either two different experiments alone in combination with other modalities such as electrical muscle stimulation (EMS), ischemic compression interferential therapy (IFT), or US.8,12-17,19,20,22,23,25-27,40
Smania et al,in their study, compared the long, medium, and short-term impacts of peripheral repetitive magnetic stimulation (rMS) and TENS on 53 patients with MPS. Their results indicate that a long-lasting impact of rMS compared to the TENS.28
In line with this result, Ardiç et al. compared the TENS and EMS on MPS on 40 patients in three different groups, including TENS + exercise, EMS + exercise, and only exercise. No statistical differences were found in any of the parameters between TENS and EMS groups at any time (P > 0.05), indicating that there is no considerable superiority of the two electrotherapies methods on each other in long term evaluation, although the effectiveness of TENS is found immediately followed by treatment.8 Another RCT was performed by Sahin et al. on the effects of TENS and reported that TENS types were not greater than other MPS treatment groups or placebo.17 Ramanathan et al compared the impact of conventional physiotherapy (TENS and Ultrasound (US)) with ischemic compression using stretching in MPS treatment. They observed that ischemic pressure was more effective than the conventional method in reducing pain.19 Rodríguez-Fernández et al showed contrary results with the application of burst-type TENS for ten minutes and concluded a small but statistically significant increase in the PPT over upper trapezius latent myofascial trigger points (MTrPs).16
Hou et al, in their RCT on 119 subjects, assessed the immediate effects of physical therapeutic modalities on myofascial pain in the upper trapezius muscle and concluded that therapeutic combinations are most operative for MPS relief like TENS, hot pack plus active ROM and stretch with spray, hot pack plus an active range of motion (ROM) and stretch with spray, as well as, hot pack plus active ROM, interferential current and myofascial release technique.15
Gemmell et al compared the results of TENS and sham on 60 MPS patients and observed that TENS was superior to placebo in reducing pain but had no better effect than placebo in improving PPT.14
Azatcam et al, in an RCT on 69 MPS patients, compared the effect of TENS + exercise, Kinesio Taping (KT) + exercise, and exercise only on the pain, and revealed a reduction in pain in all groups immediately after treatment and three months after treatment (P < 0.01). However, the VAS score was reduced in the KT group in comparison to the control group and TENS (P = 0.001), and in the TENS group compared to the control group (P = 0.011) after treatment. Considering the evaluations after 3 months and, the VAS score was reduced in the TENS group in comparison to the control group (P = 0.001), as well as in the KT group than the control group (P = 0.001). No considerable differences were found between KT and TENS groups.12 In line with the influential role of TENS in pain reduction, Dissanayaka showed that TENS with standard care facilitates had better outcomes than IFT.13 Takla investigated the effect of combination therapy with the application of US and TENS. In their trial, 70 patients underwent the burst‐TENS‐combined therapy (CT), medium-frequency, low-intensity amplitude modulated frequency (AMF)‐CT, or sham‐CT control groups. Both combination therapies effectively increased PPT.18 Other trials reported a better efficacy of TENS in combination with other modalities, including needling,25 or pharmacotherapies (methocarbamol and naproxen)23 (fluoxetine, clonazepam, baclofen)26 in comparison to needling,25 or low-level laser (LLL) approaches. However, in comparison the TENS,20,27 the efficacy of US significantly was higher. In addition, TENS on the acupuncture point was accompanied by superior improvement than the TENS on the TrP in pain intensity.22
Our meta-analysis included only the studies in which TENS was used only in the intervention arm and compared them with sham, placebo, or exercise. The only combination therapy included in our meta-analysis belonged to the combination therapy of TENS and exercise in the experimental group.15
Results of Meta-analysis
Effectiveness of TENS on VAS score
Five RCTs, including seven trials with 214 participants who evaluated the efficacy of TENS compared to placebo or control, sham or exercise, were eligible to be included in the meta-analysis.8,12,13,15,17 The scale used was VAS. However, one of them had a combination of standard care for the control arm (active ROM exercises, myofascial release, hot pack, and a home exercise program with postural advice), which was not considered in this meta-analysis.13 The I2 index represented considerable heterogeneity between studies (I2 = 88%, P value < 0.0001); thus, a random effect model was utilized to pool the data. A significant reduction was found by the overall estimated effect in VAS score in the TENS group in comparison to the exercise group (MD = -1.60, 95% CI: -2.16 to -1.05, P < 0.001). Sahin et al, had three intervention groups: Group 1 received a conventional TENS with a frequency of 100 Hz, 40 μs duration, low amplitude; Group 2 with an acupuncture-like TENS with a frequency of 4 Hz, 250 μs duration, high amplitude; Group 3 with burst TENS with high [100 Hz] and low [2 Hz] frequency, 40 μs, and high amplitude. A control group was treated with electrical stimulation until the patient felt it. The results of subgroup analysis with the control arm of sham TENS showed no statistical difference between the groups (MD: 0.45, 95% CI: -0.21 to 1.12, P = 0.18). Also, test for the overall effect of TENS compared to the control arm (either sham or exercise) did not show any significant difference between study groups (MD = -0.67, 95% CI: -1.70 to 0.36, P = 0.20). Our results also showed that TENS therapy did not ameliorate patients’ pain using the VAS scale (Figure 2).
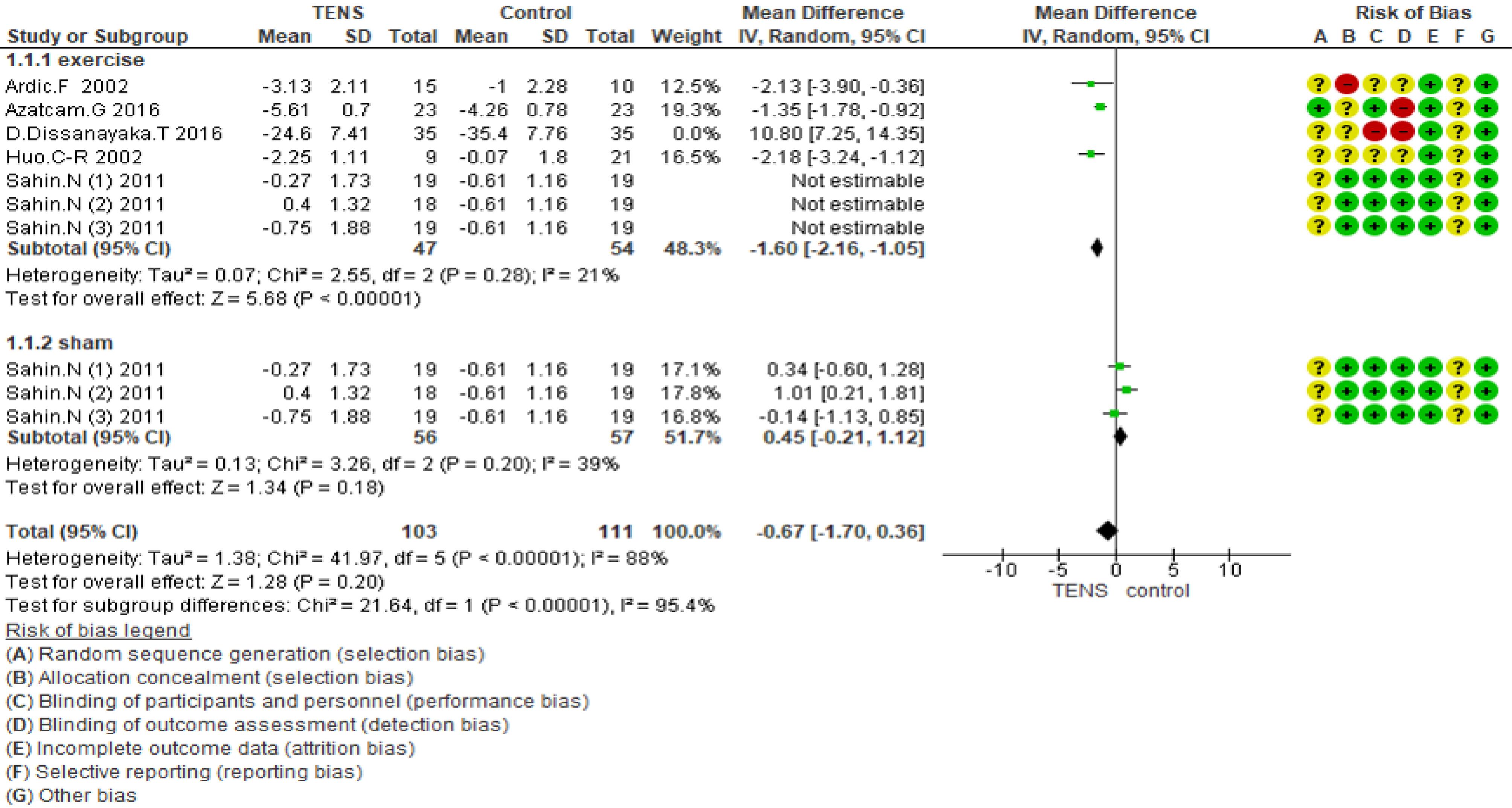
Figure 2.
Forest plot of comparison TENS vs. control on VAS score
.
Forest plot of comparison TENS vs. control on VAS score
Effectiveness of TENS on PPT score
Five RCTs involving 222 participants who evaluated the efficacy of TENS compared to placebo or control or sham or exercise were included in the meta-analysis.8,12,15,16,18,35 The scale used was PPT. The I2 index showed significant heterogeneity between studies (I2 = 99%, P < 0.00001), and therefore a random effect model was used to pool the data. The overall estimated effect showed no significant decrease in PPT score in the TENS group compared with sham (MD = 1.88, 95% CI: -0.62 to 4.38, P = 0.14) or exercise (MD = 0.19, 95% CI: -0.99 to 1.37, P = 0.75). In total, TENS therapy did not improve the PPT score (MD = 0.96, 95% CI: -0.72 to 2.64, P = 0.26) (Figure 3).
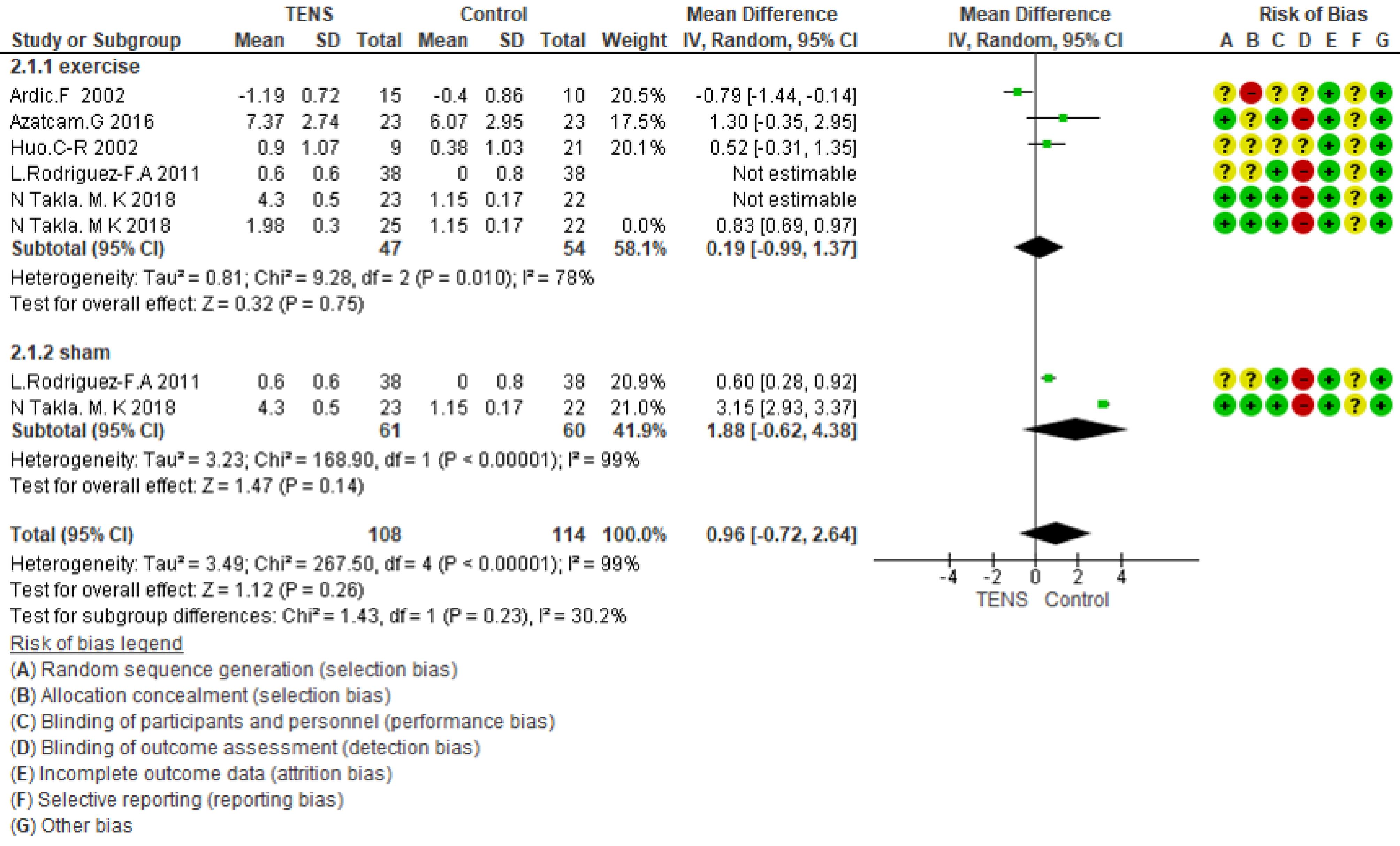
Figure 3.
Forest plot of comparison TENS vs. control on PPT score
.
Forest plot of comparison TENS vs. control on PPT score
Discussion
MPS is poorly understood and remains a challenging condition to treat. Effective management of MPS is to diagnose it early, subsequently intensive, protocol-based, multi-disciplinary rehabilitation applying a combination of medication, rest, physiotherapy, and effective use of various trigger point management techniques. Myofascial pain is typically treated by interventions directed at modifying trigger point sensitivity.36 The primary objective of treatment is to resolve the pathologic conditions of MPS. Reducing the disability and pain are the secondary treatment objectives.37 TENS is efficient, safe, and a relatively simple physical modality usually utilized in painful conditions. The TENS devices lead to patients less dependence to analgesics and narcotics.38 The present work reviewed all available evidence from RCTs and quasi RCTs systematically to summarize the effects of TENS on pain scores in myofascial pain. The use of the TENS in the management of MPS has been well-established, previously. In this regard, a study conducted by Wessberg et al, reported a much higher rate of pain reduction (95%) in patients with myofascial pain.39 Kruger et al in 1998 determined that in treating chronic pain, the application of TENS has been proposed as a practical adjunct modality.40 Additionally, it has been reported that 63.6% of patients with myalgia were completely relieved of pain after receiving TENS therapy, while another study reported that 23.3% of patients were pain-free following TENS.41,42
To date, data about the comparison of different TENS protocols in the tr0eatment of MPS are limited.17,18 On the other hand, the studies regarding the efficacy of TENS in the treatment of MPS are conflicting.7,16,17 Moreover, a recent systematic review also found that TENS is effective for the treatment of MPS.43 As stated by the present study, TENS is superior to placebo in pain reduction and pain perception improvement. TENS can decrease pain severity and increase pain threshold in MPS patients, as well.
According to the clinical studies using TENS at various frequencies, moderate to high TENS frequencies (20-80 Hz), are most effective to reduce pain intensity regarding high frequencies i.e.,100 Hz or low frequencies < 10 Hz in both clinical and healthy subjects.44 The findings also showed primary evidence that treatment sessions with durations higher than 15 min have more effectiveness compared to the short-duration sessions.43
In general, TENS was beneficial among the noninvasive therapeutic modalities.37 The difference in pain reduction in the mentioned studies is ascribed to the difference between the samples with regard to variations in biological and social constituents affecting the MPS, along with the stimulation parameters used in the TENS therapy.
Study limitations
Several limitations are present in this study. Only seven studies were included in the meta-analysis. However, all of the included studies were RCTs, and we performed a quality assessment of the risk of bias to overcome this limitation. All studies included in this analysis possessed a relatively small sample size. It must be highlighted that the duration of therapeutic effect and effect sizes are often limited; therefore, real clinical impact should be determined with further large-scaled clinical research.
Conclusion
This manuscript reviewed the main aspects of TENS on pain scores in myofascial pain. Thus, TENS can be utilized as an adjuvant treatment to help alleviate MPS but should not be regarded as a monotherapy. The results of trials were heterogeneous because of large variability within the applied parameters and protocols. The limited sample size and poor quality of these studies highlight and support the need for additional studies with larger numbers of participants, and good quality placebo-controlled trials in this area.
Acknowledgments
The authors would like to thank the Physical Medicine and Rehabilitation Research Center, Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran, and the Evidence-based Medical Research Center, Tabriz University of Medical Sciences, Tabriz, Iran for supporting this work.
Competing Interests
There is no conflict of interest.
Ethical Approval
The current study was approved by the Research Ethics Committee of the Tabriz University of Medical Science (No: IR.TBZMED.REC.1400.926).
References
- Saxena A, Chansoria M, Tomar G, Kumar A. Myofascial pain syndrome: an overview. J Pain Palliat Care Pharmacother 2015; 29(1):16-21. doi: 10.3109/15360288.2014.997853 [Crossref] [ Google Scholar]
- Urits I, Charipova K, Gress K, Schaaf AL, Gupta S, Kiernan HC. Treatment and management of myofascial pain syndrome. Best Pract Res Clin Anaesthesiol 2020; 34(3):427-48. doi: 10.1016/j.bpa.2020.08.003 [Crossref] [ Google Scholar]
- Fredy DM, Harpin D, Mihardja H. The role of acupuncture for myofascial pain syndrome (MPS) in interventional pain management. J Complement Integr Med 2022; 19(2):213-217. doi: 10.1515/jcim-2021-0525 [Crossref] [ Google Scholar]
- Cao QW, Peng BG, Wang L, Huang YQ, Jia DL, Jiang H. Expert consensus on the diagnosis and treatment of myofascial pain syndrome. World J Clin Cases 2021; 9(9):2077-89. doi: 10.12998/wjcc.v9.i9.2077 [Crossref] [ Google Scholar]
- Galasso A, Urits I, An D, Nguyen D, Borchart M, Yazdi C. A comprehensive review of the treatment and management of myofascial pain syndrome. Curr Pain Headache Rep 2020; 24(8):43. doi: 10.1007/s11916-020-00877-5 [Crossref] [ Google Scholar]
- Martimbianco ALC, Porfírio GJ, Pacheco RL, Torloni MR, Riera R. Transcutaneous electrical nerve stimulation (TENS) for chronic neck pain. Cochrane Database Syst Rev 2019; 12(12):CD011927. doi: 10.1002/14651858.CD011927.pub2 [Crossref] [ Google Scholar]
- Vance CG, Dailey DL, Rakel BA, Sluka KA. Using TENS for pain control: the state of the evidence. Pain Manag. 2014 May;4(3):197-209. 10.2217/pmt.14.13.
- Ardiç F, Sarhus M, Topuz O. Comparison of two different techniques of electrotherapy on myofascial pain. J Back Musculoskelet Rehabil 2002; 16(1):11-6. doi: 10.3233/bmr-2002-16103 [Crossref] [ Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009; 339:b2700. doi: 10.1136/bmj.b2700 [Crossref] [ Google Scholar]
- Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 2019; 10(10):ED000142. doi: 10.1002/14651858.ed000142 [Crossref] [ Google Scholar]
- Fu R, Vandermeer BW, Shamliyan TA, O’Neil ME, Yazdi F, Fox SH, et al. AHRQ methods for effective health care. Handling continuous outcomes in quantitative synthesis. In: Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Rockville, MD: Agency for Healthcare Research and Quality (US); 2008.
- Azatcam G, Atalay NS, Akkaya N, Sahin F, Aksoy S, Zincir O. Comparison of effectiveness of Transcutaneous Electrical Nerve Stimulation and Kinesio Taping added to exercises in patients with myofascial pain syndrome. J Back Musculoskelet Rehabil 2017; 30(2):291-8. doi: 10.3233/bmr-150503 [Crossref] [ Google Scholar]
- Dissanayaka TD, Pallegama RW, Suraweera HJ, Johnson MI, Kariyawasam AP. Comparison of the effectiveness of transcutaneous electrical nerve stimulation and interferential therapy on the upper trapezius in myofascial pain syndrome: a randomized controlled study. Am J Phys Med Rehabil 2016; 95(9):663-72. doi: 10.1097/phm.0000000000000461 [Crossref] [ Google Scholar]
- Gemmell H, Hilland A. Immediate effect of electric point stimulation (TENS) in treating latent upper trapezius trigger points: a double blind randomised placebo-controlled trial. J Bodyw Mov Ther 2011; 15(3):348-54. doi: 10.1016/j.jbmt.2010.04.003 [Crossref] [ Google Scholar]
- Hou CR, Tsai LC, Cheng KF, Chung KC, Hong CZ. Immediate effects of various physical therapeutic modalities on cervical myofascial pain and trigger-point sensitivity. Arch Phys Med Rehabil 2002; 83(10):1406-14. doi: 10.1053/apmr.2002.34834 [Crossref] [ Google Scholar]
- Rodríguez-Fernández AL, Garrido-Santofimia V, Güeita-Rodríguez J, Fernández-de-Las-Peñas C. Effects of burst-type transcutaneous electrical nerve stimulation on cervical range of motion and latent myofascial trigger point pain sensitivity. Arch Phys Med Rehabil 2011; 92(9):1353-8. doi: 10.1016/j.apmr.2011.04.010 [Crossref] [ Google Scholar]
- Sahin N, Albayrak I, Ugurlu H. Effect of different transcutaneous electrical stimulation modalities on cervical myofascial pain syndrome. J Musculoskelet Pain 2011; 19(1):18-23. doi: 10.3109/10582452.2010.538825 [Crossref] [ Google Scholar]
- Takla MK. Low-frequency high-intensity versus medium-frequency low-intensity combined therapy in the management of active myofascial trigger points: a randomized controlled trial. Physiother Res Int 2018; 23(4):e1737. doi: 10.1002/pri.1737 [Crossref] [ Google Scholar]
- Ramanathan K, Nathan CS, Kumar GM, Rajavel R. Effect of conventional physiotherapy [tens and ultrasound] vs ischemic compression with stretching in the treatment of active myofascial trigger points for upper back. J Physiother Occup Ther 2015; 1(2):7-13. [ Google Scholar]
- Amjad F, Shahid HA, Batool S, Ahmad A, Ahmed I. A comparison on efficacy of transcutaneous electrical nerve stimulation and therapeutic ultrasound in treatment of myofascial trigger points. Khyber Med Univ J 2016; 8(1):3-6. [ Google Scholar]
- Chalkoo AH, Nazir N. Evaluation of conventional therapy, transcutaneous electric nerve stimulation therapy, and placebo in management of myofascial pain-dysfunction syndrome: a comparative study. J Adv Clin Res Insights 2016; 3(2):51-5. doi: 10.15713/ins.jcri.105 [Crossref] [ Google Scholar]
- Chiou YF, Yeh ML, Wang YJ. Transcutaneous electrical nerve stimulation on acupuncture points improves myofascial pain, moods, and sleep quality. Rehabil Nurs 2020; 45(4):225-33. doi: 10.1097/rnj.0000000000000198 [Crossref] [ Google Scholar]
- Khalifeh S, Rezaee E, Azizi A, Ebrahimi H. Efficacy of low-level laser versus transcutaneous electrical nerve stimulation for treatment of myofascial pain syndrome: a clinical trial. J Res Dent Maxillofac Sci 2018; 3(3):33-41. doi: 10.29252/jrdms.3.3.33 [Crossref] [ Google Scholar]
- Kim DH, Yoon KB, Park S, Jin TE, An YJ, Schepis EA. Comparison of NSAID patch given as monotherapy and NSAID patch in combination with transcutaneous electric nerve stimulation, a heating pad, or topical capsaicin in the treatment of patients with myofascial pain syndrome of the upper trapezius: a pilot study. Pain Med 2014; 15(12):2128-38. doi: 10.1111/pme.12611 [Crossref] [ Google Scholar]
- León-Hernández JV, Martín-Pintado-Zugasti A, Frutos LG, Alguacil-Diego IM, de la Llave-Rincón AI, Fernandez-Carnero J. Immediate and short-term effects of the combination of dry needling and percutaneous TENS on post-needling soreness in patients with chronic myofascial neck pain. Braz J Phys Ther 2016; 20(5):422-31. doi: 10.1590/bjpt-rbf.2014.0176 [Crossref] [ Google Scholar]
- Mansourian A, Pourshahidi S, Sadrzadeh-Afshar MS, Ebrahimi H. A comparative study of low-level laser therapy and transcutaneous electrical nerve stimulation as an adjunct to pharmaceutical therapy for myofascial pain dysfunction syndrome: a randomized clinical trial. Front Dent 2019; 16(4):256-64. doi: 10.18502/fid.v16i4.2084 [Crossref] [ Google Scholar]
- Rai S, Ranjan V, Misra D, Panjwani S. Management of myofascial pain by therapeutic ultrasound and transcutaneous electrical nerve stimulation: a comparative study. Eur J Dent 2016; 10(1):46-53. doi: 10.4103/1305-7456.175680 [Crossref] [ Google Scholar]
- Smania N, Corato E, Fiaschi A, Pietropoli P, Aglioti SM, Tinazzi M. Repetitive magnetic stimulation: a novel therapeutic approach for myofascial pain syndrome. J Neurol 2005; 252(3):307-14. doi: 10.1007/s00415-005-0642-1 [Crossref] [ Google Scholar]
- Jeon JH, Jung YJ, Lee JY, Choi JS, Mun JH, Park WY. The effect of extracorporeal shock wave therapy on myofascial pain syndrome. Ann Rehabil Med 2012; 36(5):665-74. doi: 10.5535/arm.2012.36.5.665 [Crossref] [ Google Scholar]
- Kim M, Lee M, Kim Y, Oh S, Lee D, Yoon B. Myofascial pain syndrome in the elderly and self-exercise: a single-blind, randomized, controlled trial. J Altern Complement Med 2016; 22(3):244-51. doi: 10.1089/acm.2015.0205 [Crossref] [ Google Scholar]
- Gezgİnaslan Ö, Gümüş Atalay S. High-energy flux density extracorporeal shock wave therapy versus traditional physical therapy modalities in myofascial pain syndrome: a randomized-controlled, single-blind trial. Arch Rheumatol 2020; 35(1):78-89. doi: 10.5606/ArchRheumatol.2020.7496 [Crossref] [ Google Scholar]
- Kim M, Lee M, Kim Y, Oh S, Lee D, Yoon B. Myofascial pain syndrome in the elderly and self-exercise: a single-blind, randomized, controlled trial. J Altern Complement Med 2016; 22(3):244-51. doi: 10.1089/acm.2015.0205 [Crossref] [ Google Scholar]
- Dissanayake TD, Kariyawasam A, Pallegama RW, Suraweera HJ, Dassanayake T. Immediate Effectiveness of Transcutaneoue Electrical Nerve Stimulation (Tens) in Treating Trigger Points of the Upper Trapezius in Myofascial Pain Syndrome: A Preliminary Study. Sri Lanka: University of Peradeniya; 2013.
- Jeon JH, Jung YJ, Lee JY, Choi JS, Mun JH, Park WY. The effect of extracorporeal shock wave therapy on myofascial pain syndrome. Ann Rehabil Med 2012; 36(5):665-74. doi: 10.5535/arm.2012.36.5.665 [Crossref] [ Google Scholar]
- Takla MK, Rezk-Allah SS. Immediate effects of simultaneous application of transcutaneous electrical nerve stimulation and ultrasound phonophoresis on active myofascial trigger points: a randomized controlled trial. Am J Phys Med Rehabil 2018; 97(5):332-8. doi: 10.1097/phm.0000000000000876 [Crossref] [ Google Scholar]
- Gerwin RD. Diagnosis of myofascial pain syndrome. Phys Med Rehabil Clin 2014; 25(2):341-55. doi: 10.1016/j.pmr.2014.01.011 [Crossref] [ Google Scholar]
- Desai MJ, Bean MC, Heckman TW, Jayaseelan D, Moats N, Nava A. Treatment of myofascial pain. Pain Manag 2013; 3(1):67-79. doi: 10.2217/pmt.12.78 [Crossref] [ Google Scholar]
- Vasudev S, Vakade CD, Paramesh RC, Govind BP. Transcutaneous electric nerve stimulation: an adjuvant modality for pain relief in myofascial pain dysfunction syndrome. J Med Radiol Pathol Surg 2017; 4(4):9-11. [ Google Scholar]
- Wessberg GA, Carroll WL, Dinham R, Wolford LM. Transcutaneous electrical stimulation as an adjunct in the management of myofascial pain-dysfunction syndrome. J Prosthet Dent 1981; 45(3):307-14. doi: 10.1016/0022-3913(81)90396-6 [Crossref] [ Google Scholar]
- Kruger LR, van der Linden WJ, Cleaton-Jones PE. Transcutaneous electrical nerve stimulation in the treatment of myofascial pain dysfunction. S Afr J Surg 1998; 36(1):35-8. [ Google Scholar]
- Patil S, Iyengar AR, Kotni RM, B VS, Joshi RK. Evaluation of efficacy of ultrasonography in the assessment of transcutaneous electrical nerve stimulation in subjects with myositis and myofascial pain. Korean J Pain 2016; 29(1):12-7. doi: 10.3344/kjp.2016.29.1.12 [Crossref] [ Google Scholar]
- Moger G, Shashikanth MC, Sunil MK, Shambulingappa P. Transcutaneous electrical nerve stimulation therapy in temporomandibular disorder: a clinical study. J Indian Acad Oral Med Radiol 2011; 23(1):46-50. doi: 10.5005/jp-journals-10011-1090 [Crossref] [ Google Scholar]
- Ahmed S, Haddad C, Subramaniam S, Khattab S, Kumbhare D. The effect of electric stimulation techniques on pain and tenderness at the myofascial trigger point: a systematic review. Pain Med 2019; 20(9):1774-88. doi: 10.1093/pm/pny278 [Crossref] [ Google Scholar]
- Johnson MI, Ashton CH, Bousfield DR, Thompson JW. Analgesic effects of different frequencies of transcutaneous electrical nerve stimulation on cold-induced pain in normal subjects. Pain 1989; 39(2):231-6. doi: 10.1016/0304-3959(89)90010-9 [Crossref] [ Google Scholar]